Jun. 16, 2020
So many people Seth Marder spoke to didn’t see the hand sanitizer crisis brewing. The country was going to run dangerously short if someone did not act urgently.
The professor at the Georgia Institute of Technology rallied colleagues and partners around the cause in March, and by early June, they had replaced a key component of hand sanitizer, created a new supply chain, and initiated their own donation of 7,000 gallons of a newly designed sanitizer to medical facilities.
Its name: Han-I-Size White & Gold, named for the colors of Georgia Tech. The new supply chain also may ensure that hand sanitizer producers across the country do not run out of the main active ingredient, alcohol, but the team’s path to success was a stony labyrinth.
“This project was on life support so many times because people did not understand how severe this shortage was going to be,” said Marder, a Regents Professor in Georgia Tech’s School of Chemistry and Biochemistry. “I called hospitals and institutions to assess the need and heard the same thing over and over: ‘No, we just got a delivery. We have no need. You’re wasting your time.’”
Marder was not. Contacts at major chemical suppliers of hand sanitizer ingredients said that a critical shortage of alcohol, particularly the one usually in hand sanitizer, isopropanol, was coming.
“Isopropanol plants in the U.S. were running at full capacity and still didn’t have enough. People were using pharmaceutical-grade ethanol now, too, but it was also in short supply. We weren’t going to have enough of either; I mean the whole United States was running low,” Marder said.
Clean hands cabal
Marder hastily drafted Chris Luettgen, a professor of practice in Georgia Tech’s School of Chemical and Biomolecular Engineering, George White, interim vice president of Georgia Tech’s Office of Industry Collaboration, and Atif Dabdoub, a Georgia Tech alumnus and owner of a local chemical company, Unichem Technologies, Inc.
To the three chemists and the business professional, it seemed simple: Mix alcohol with water, peroxide, and the moisturizer glycerin then bottle and ship it. That bubble burst quickly.
Luettgen, who had worked in the consumer products industry for 25 years at Kimberly-Clark Corporation and knew how to take products to market, had to plow through constant unexpected supply chain barriers and bureaucracy while White forged connections between companies. Neither the supply chain nor the business relationships had existed before, and the teams’ phones stayed glued to their ears night and day as they created them from scratch.
“When I worked for Kimberly-Clark, getting a new product out would take the company nine to 18 months, and the three of us had to get this done in weeks. The demand was there, and people were getting sick in some cases from lack of sanitizing. We felt speed was necessary to meet the growing demand. Seth told me to push this across the goal line, and I put everything into it,” Luettgen said.
“Georgia Tech is about the power to convene. Companies and stakeholders are eager to come to the table here to make things happen,” White said about forging new business ties. “Not everyone has that incredible recognition as a problem solver with the brainpower amassed here.”
Stinking of gin
Purchasing truckloads of alcohol was priority one.
Boutique liquor distilleries in Georgia were already converting to sanitizer ethyl alcohol production, but output was nowhere near enough to meet demand. ExxonMobil connected the team with Eco-Energy, a company that handles fuel-grade ethanol as a gasoline additive.
“The amount of ethanol that’s made for fuel in the U.S. is 1,500 times the amount of the isopropanol made. They could drain off about 1 percent of what is used for fuel and double or triple the amount of alcohol available for hand sanitizer in this country. And the fuel companies wouldn’t even notice it was gone, especially since hardly anyone was driving anymore,” Marder said.
But then prospective hand sanitizer distributors crimped their noses at that ethanol, saying it smelled odd.
“I thought, ‘This has the makings of a screenplay.’ I asked the distributor if we could come over to smell a sample for ourselves,” White said. “It needed a little love.”
Eco-Fuels produced the highly refined ethanol and then processed it through carbon filtration to increase purity and reduce odor. Atlanta-based chemical manufacturer, Momar, Inc., oversaw production, packaging, and distribution of Han-I-Size White & Gold.
The Georgia Tech team garnered funding through a donation from insurer Aflac Incorporated allocated through the Global Center for Medical Innovation (GCMI), a Georgia Tech affiliated non-profit organization that guides new experimental medical solutions to market. Aflac’s gift of $2 million through GCMI has also expedited the development, production, and purchase of other PPE to donate to health care workers.
In addition, GCMI helped guide the hand sanitizer through regulatory processes and to market. In a another development, the U.S. Food and Drug Administration was also aware of the dire shortage of alcohol for sanitizer and issued waivers for the pandemic to allow for use of ethanol in sanitizers without having to meet usual specifications.
Water, water everywhere
Arkema, Inc. donated hydrogen peroxide, which was delivered to PSG Functional Materials, which mixed and packaged the product then shipped with no delivery fee to Atlanta. Though water is ubiquitous, hand sanitizer requires purified water, and the Coca-Cola Company donated a tanker truck of it just when White was pondering desperate measures.
“If I have to get a truck to go pick up water and drive it, I’ll do it myself,” he said.
Finally, the first few hundred gallons of donated Han-I-Size White & Gold rolled into Piedmont Healthcare in Atlanta and Brightmoor Nursing Center in Griffin, Georgia, in the second week of June 2020.
GCMI is facilitating donations of the 7,000 gallons nationwide. Separate from the Aflac-financed donations, Momar will continue to manufacture the new hand sanitizing formula commercially to include in its regular product lineup, and Georgia Tech will be able to purchase it at a reduced rate to help protect researchers now returning to their labs.
The new supply chain, the first of its kind, of “waiver-grade” ethanol has given hand sanitizer producers across the country a new opportunity to re-supply America.
“Hopefully, we helped solved a national need,” Luettgen said.
Read about what else we are doing to help in the Covid-19 crisis.
Here's how to subscribe to our free science and technology email newsletter
Writer & media inquiries: Ben Brumfield, ben.brumfield@comm.gatech.edu or John Toon (404-894-6986), jtoon@gatech.edu.
Georgia Institute of Technology
May. 07, 2020
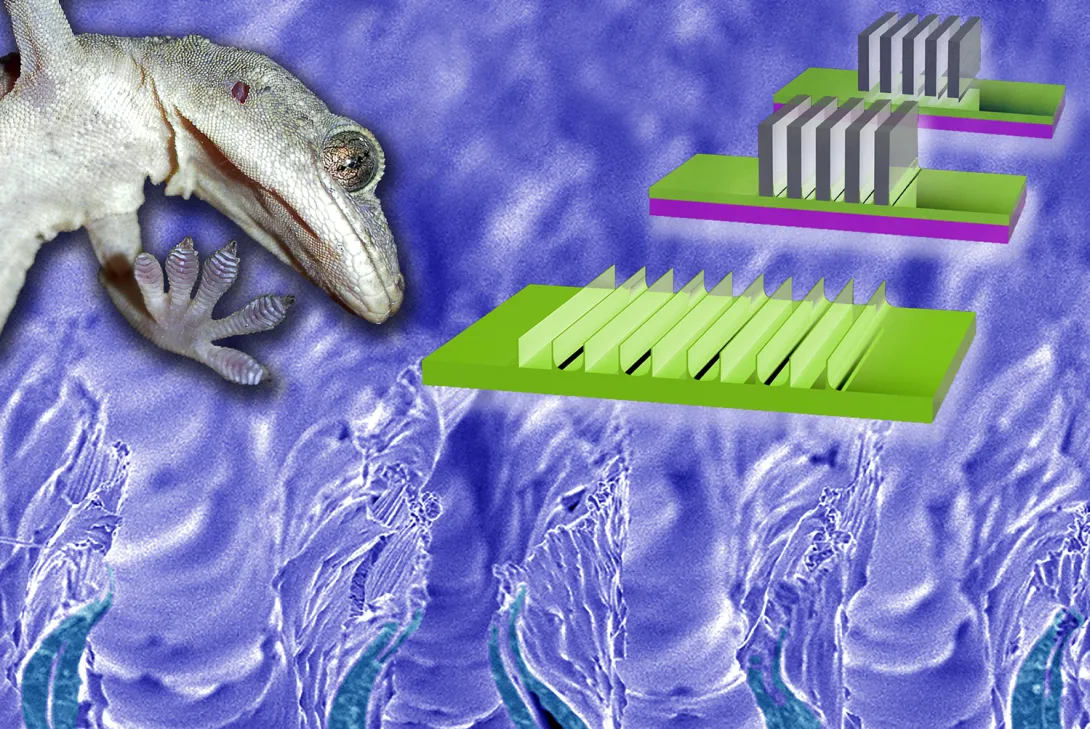
Why did the gecko climb the skyscraper? Because it could; its toes stick to about anything. Engineers can already emulate the secrets of gecko stickiness to make strips of rubbery materials that can pick up and release objects, but simple mass production for everyday use has been out of reach until now.
Researchers at the Georgia Institute of Technology have developed, in a new study, a method of making gecko-inspired adhesive materials that is much more cost-effective than current methods. It could enable mass production and the spread of the versatile gripping strips to manufacturing and homes.
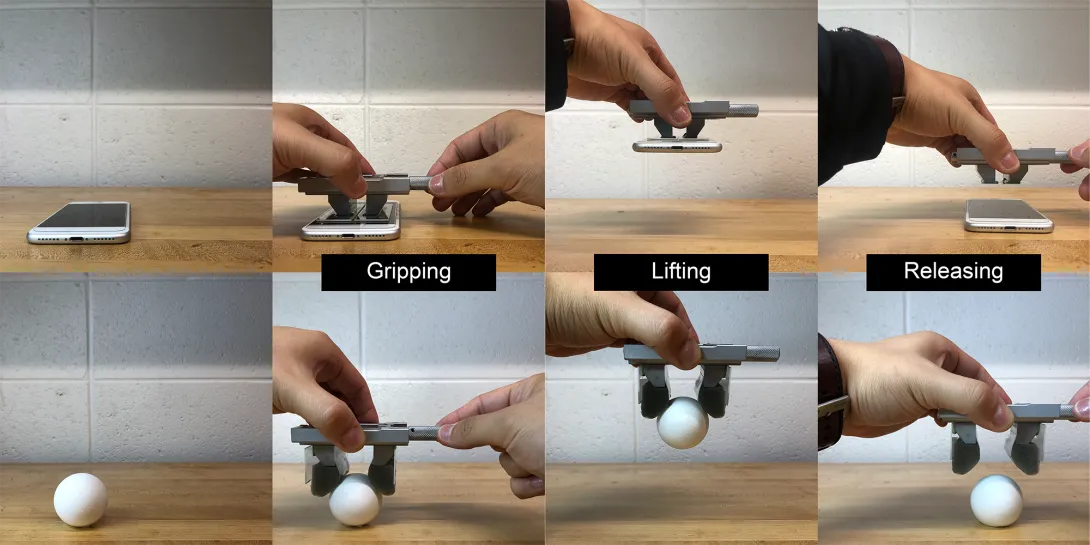
Polymers with “gecko adhesion” surfaces could be used to make extremely versatile grippers to pick up very different objects even on the same assembly line. They could make picture hanging easy by adhering to both the picture and the wall at the same time. Vacuum cleaner robots with gecko adhesion could someday scoot up tall buildings to clean facades.
“With the exception of things like Teflon, it will adhere to anything. This is a clear advantage in manufacturing because we don’t have to prepare the gripper for specific surfaces we want to lift. Gecko-inspired adhesives can lift flat objects like boxes then turn around and lift curved objects like eggs and vegetables,” said Michael Varenberg, the study’s principal investigator and an assistant professor in Georgia Tech’s George W. Woodruff School of Mechanical Engineering.
Current grippers on assembly lines, such as clamps, magnets, and suction cups, can each lift limited ranges of objects. Grippers based on gecko-inspired surfaces, which are dry and contain no glue or goo, could replace many grippers or just fill in capability gaps left by other gripping mechanisms.
Drawing out razors
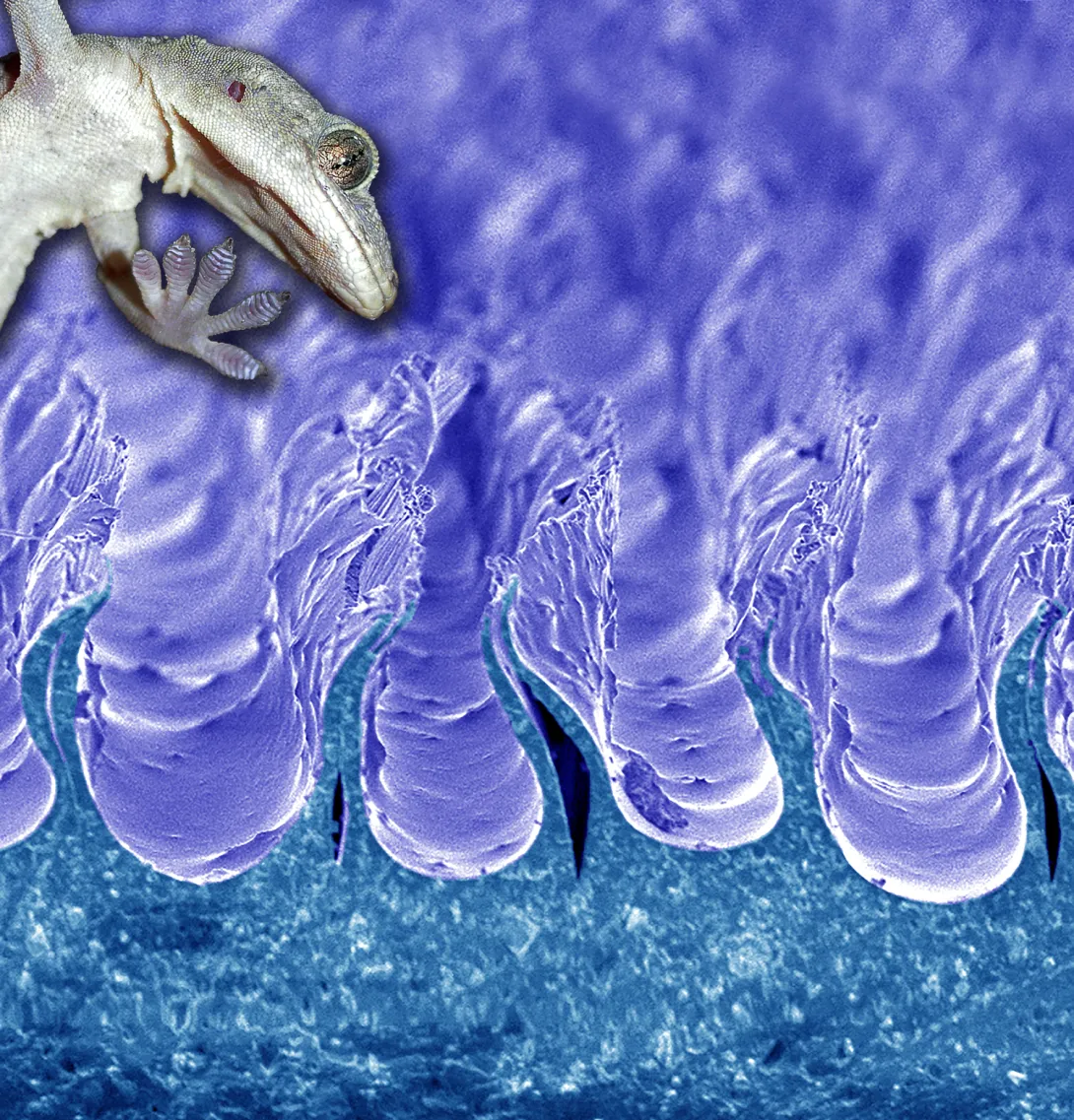
The adhesion comes from protrusions a few hundred microns in size that often look like sections of short, floppy walls running parallel to each other across the material’s surface. How they work by mimicking geckos’ feet is explained below.
Up to now, molding has produced these mesoscale walls by pouring ingredients onto a template, letting the mixture react and set to a flexible polymer then removing it from the mold. But the method is inconvenient.
“Molding techniques are expensive and time-consuming processes. And there are issues with getting the gecko-like material to release from the template, which can disturb the quality of the attachment surface,” Varenberg said.
The researchers’ new method formed those walls by pouring ingredients onto a smooth surface instead of a mold, letting the polymer partially set then dipping rows of laboratory razor blades into it. The material set a little more around the blades, which were then drawn out, leaving behind micron-scale indentations surrounded by the desired walls.
Varenberg and first author Jae-Kang Kim published details of their new method in the journal ACS Applied Materials & Interfaces on April 6, 2020.
Forget about perfection
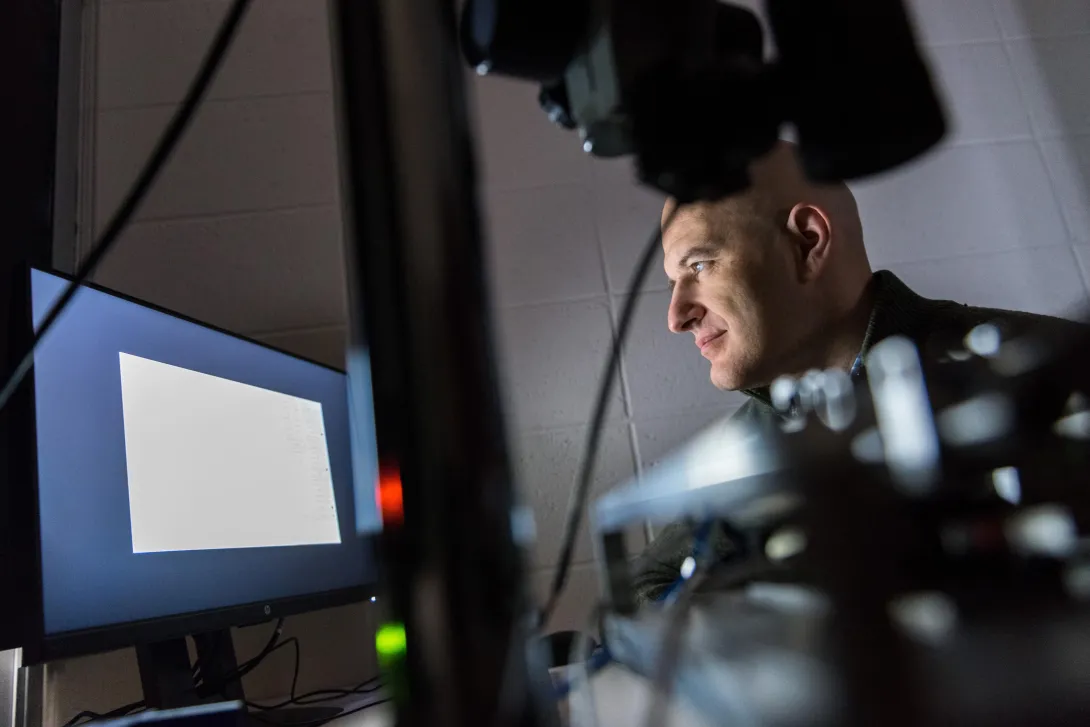
Though the new method is easier than molding, developing it took a year of dipping, drawing, and readjusting while surveying finicky details under an electron microscope.
“There are many parameters to control: Viscosity and temperature of the liquid; timing, speed, and distance of withdrawing the blades. We needed enough plasticity of the setting polymer to the blades to stretch the walls up, and not so much rigidity that would lead the walls to rip up,” Varenberg said.
Gecko-inspired surfaces have a fine topography on a micron-scale and sometimes even on a nanoscale, and surfaces made via molding are usually the most precise. But such perfection is unnecessary; the materials made with the new method did the job well and were also markedly robust.
“Many researchers demonstrating gecko adhesion have to do it in a cleanroom in clean gear. Our system just plain works in normal settings. It is robust and simple, and I think it has good potential for use in industry and homes,” said Varenberg, who studies surfaces in nature to mimic their advantageous qualities in human-made materials.
[Ready for graduate school with social distancing? Here's how to apply to Georgia Tech.]
Gecko foot fluff
Behold the gecko’s foot. It has ridges on its toes, and this has led some in the past to think their feet stick by suction or some kind of clutching by the skin.
But electron microscopes reveal a deeper structure – spatula-shaped bristly fibrils protrude a few dozen microns long off those ridges. The fibrils make such thorough contact with surfaces down to the nanoscale that weak attractions between atoms on both sides appear to add up enormously to create overall strong adhesion.
In place of fluff, engineers have developed rows of shapes covering materials that produce the effect. A common shape makes a material’s surface look like a field of mushrooms that are a few hundred microns in size; another is rows of short walls like those in this study.
“The mushroom patterns touch a surface, and they are attached straightaway, but detaching requires applying forces that can be disadvantageous. The wall-shaped projections require minor shear force like a tug or a gentle grab to generate adherence, but that is easy, and letting go of the object is uncomplicated, too,” Varenberg said.
Varenberg’s research team used the drawing method to make walls with U-shaped spaces in between them and walls with V-shaped spaces in between. They worked with polyvinylsiloxane (PVS) and polyurethane (PU). The V-shape made in PVS worked best, but polyurethane is the better material for industry, so Vanenberg’s group will now work toward achieving the V-shape gecko gripping pattern in PU for the best possible combination.
Also read: Lung-heart super sensor on a chip tinier than a ladybug
Here's how to subscribe to our free science and technology email newsletter
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 22, 2020
Gaps in the supply of coronavirus tests are propelling initiatives to fill them across the country. At the Georgia Institute of Technology, bioscience researchers are burning the midnight oil to produce key components for tests in the state of Georgia.
The goal is to supply a broad initiative by the governor’s office involving multiple universities and partners to rapidly produce and administer more tests. At least 35 volunteers at Georgia Tech, while adhering to social distancing, are reorienting labs normally used for scientific discovery to do larger-scale production of biochemical components.
“We are inventing new ways of doing things like an electronic buddy system so people can be alone – but not alone – while they work in the lab. The technical part is actually the easiest. The logistics of testing, data security, and regulatory considerations – those things are more challenging,” said Loren Williams, a professor in Georgia Tech’s School of Chemistry and Biochemistry.
Williams and the researchers are supporting Georgia Governor Brian Kemp’s COVID-19 State Lab Surge Capacity Task Force, which is a project managed through the Georgia Tech Research Institute (GTRI). GTRI is also leading the coordination and integration of data management across the lab surge effort.
“We are providing technical and project management of the effort which is focused on increasing the state’s ability to expand testing beyond current limitations,” said Mike Shannon, GTRI’s lead in the project and a principal research engineer at GTRI.
Exoplanets and coronavirus
The science behind coronavirus testing is complementary to the researchers’ usual work. That includes understanding proteins associated with glaucoma, figuring out how RNA and DNA evolved in the first place, or whether ribosomes – lumps of RNA and protein key to translating genetic code into life – may exist on exoplanets.
Williams’ research team studies the last topic, and some of their work is related to the core of coronavirus testing, a chemical reaction that amplifies the virus’ genetic fingerprint. It is called a reverse transcription polymerase chain reaction (RT-PCR), and it transcribes trace amounts of coronavirus’ RNA code into ample amounts of corresponding DNA in the lab for easy analysis.
“His lab members are very familiar with RT-PCR, and when the lack of tests became apparent, they swung into action. The group grew from there, based on the technical needs for the project,” said Raquel Lieberman, another leading scientist in the effort and also a professor in Georgia Tech’s School of Chemistry and Biochemistry.
“Every day, very talented, hardworking people with perfect skill sets come out of the woodwork and ask to help,” Williams said.
The group has teams that engineer the production of enzymes or other chemicals needed for RT-PCR to work: Two central enzymes are reverse transcriptase, which converts RNA to DNA and Taq polymerase, which rapidly replicates DNA. Another important component is ribonuclease inhibitor, which slows coronavirus RNA decay.
Global COVID allies
Other researchers develop processes for mass production or implementation of COVID-19 safety procedures; the list goes on. Some colleagues telework; others work in labs but spaced far from each other while they wear masks.
“The group is planning to produce enough enzyme components for hundreds of tests per day,” said Vinayah Agarwal, an assistant professor in Georgia Tech’s School of Chemistry and Biochemistry and School of Biological Sciences. “Using these components, we will also build cheaper and more robust testing kits going forward.”
Instructions already exist for some of the ingredients for the test, but they are not readily available because the rights to them are exclusive.
“Intellectual property and other proprietary issues hinder our effort,” Lieberman said. “But we have received help from scientists all over the world to piece together protocols on how to make what we need.”
The state wants to increase current testing capacities by 3,000 more tests per day. The task force also includes teams from Augusta University Health System, Georgia State University, Emory University, University of Georgia, and the Georgia Public Health Laboratory. The task force lead is Captain Kevin Caspary who is with the Georgia National Guard.
Raw footage and images as press handouts for journalists. (No commercial or personal use):
https://www.dropbox.com/sh/f2wc2i74lz1lffl/AADLJ8dQnZMr4uEDxAiIMusoa?dl=0
Also read this: Interactive COVID-19 tool shows the importance of staying at home
External News Coverage:
NPR - Sun Rays, Disinfectants And False Hopes: Misinformation Litters The Road To Reopening
News-Medical.Net - Georgia Tech researchers create key components for COVID-19 tests
Georgia Tech News Center- A New Normal: Researchers Across Georgia Tech Rally to Fight COVID-19
Here's how to subscribe to our free science and technology email newsletter
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 15, 2020
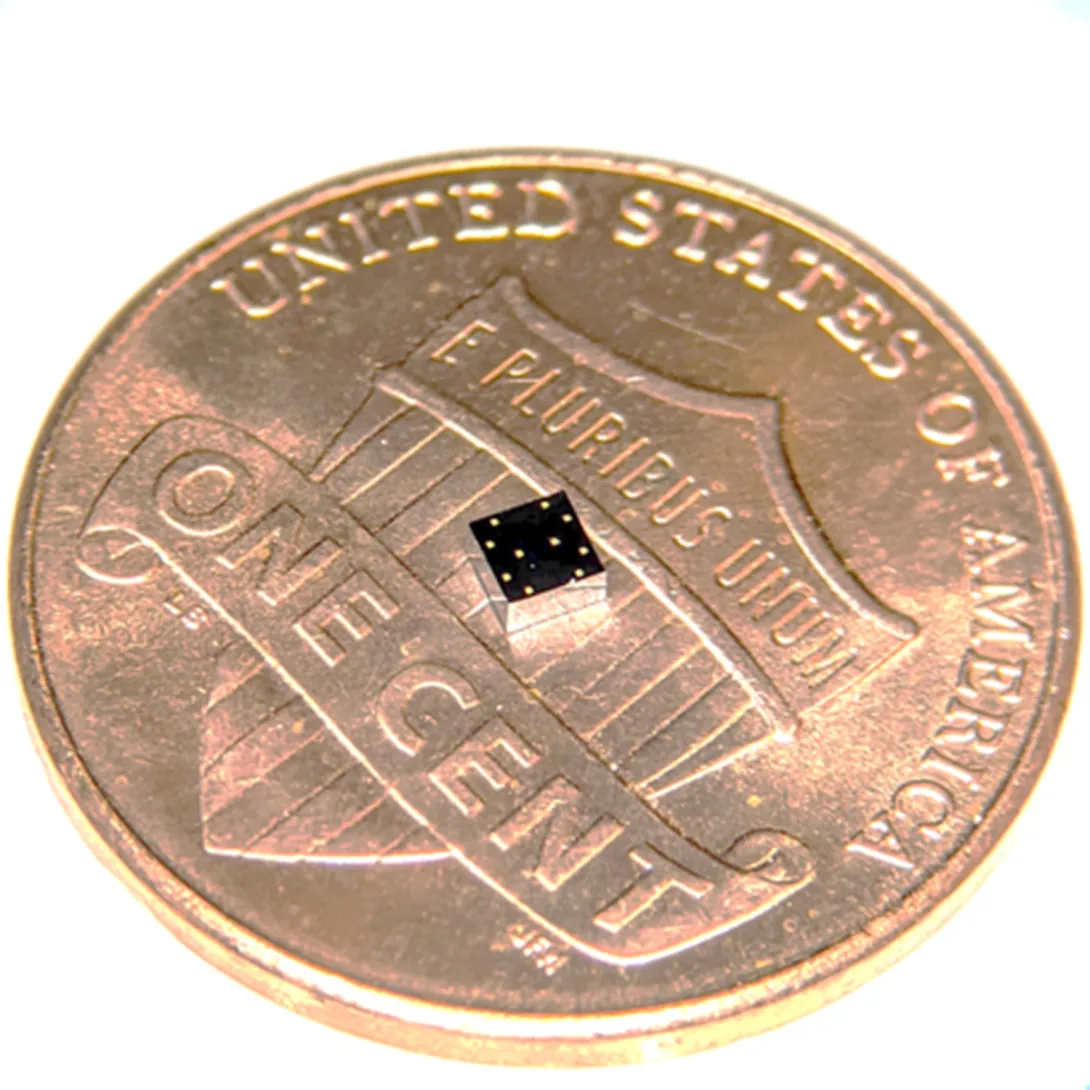
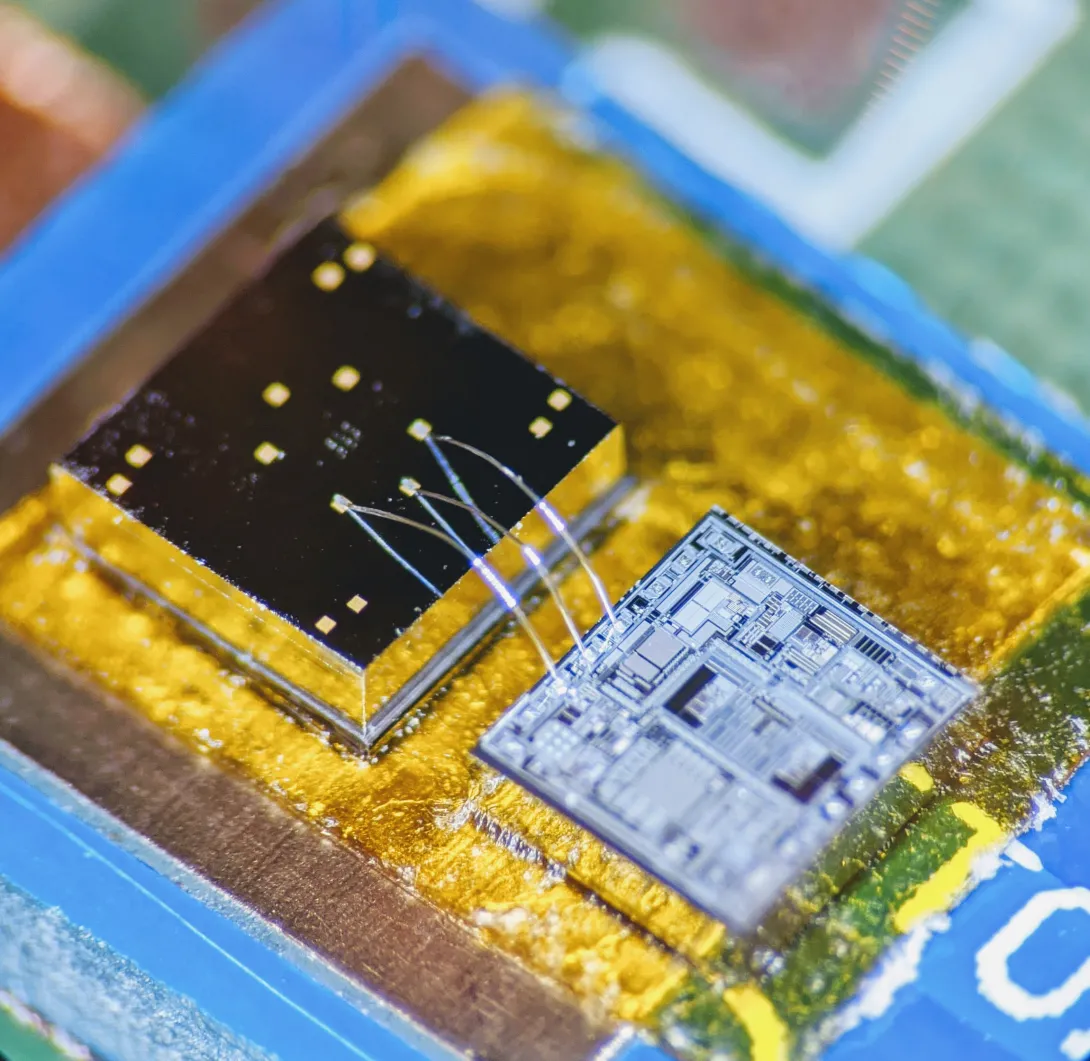
During a stroll, a woman’s breathing becomes a slight bit shallower, and a monitor in her clothing alerts her to get a telemedicine check-up. A new study details how a sensor chip smaller than a ladybug records multiple lung and heart signals along with body movements and could enable such a future socially distanced health monitor.
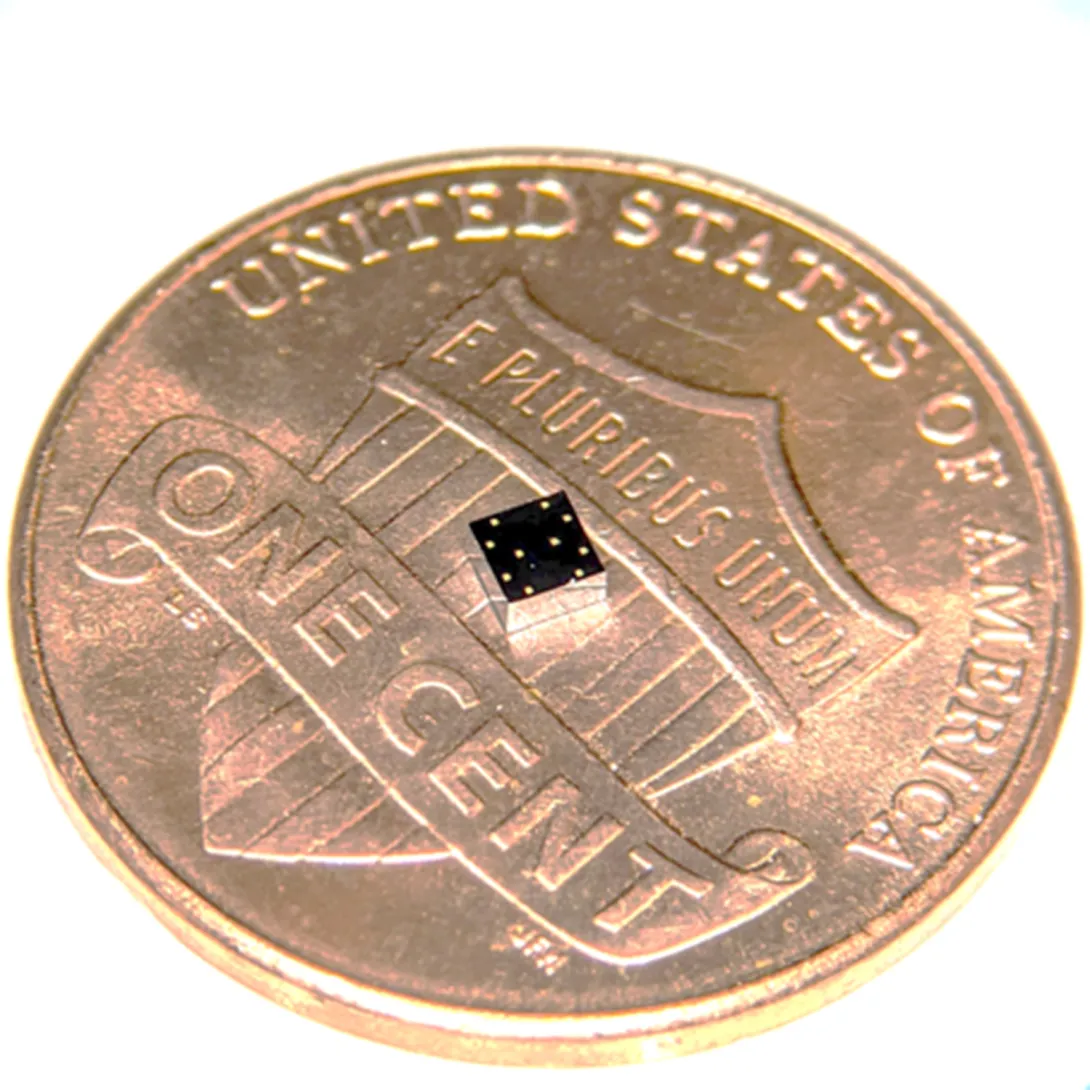
The core mechanism of the chip developed by researchers at the Georgia Institute of Technology involves two finely manufactured layers of silicon, which overlay each other separated by the space of 270 nanometers – about 0.000001 inches. They carry a minute voltage.
Vibrations from bodily motions and sounds put part of the chip in very slight motion, making the voltage flux, thus creating readable electronic outputs. In human testing, the chip has recorded a variety of signals from the mechanical workings of the lungs and the heart with clarity, signals that often escape meaningful detection by current medical technology.
“Right now, medicine looks to EKGs (electrocardiograms) for information on the heart, but EKGs only measure electrical impulses. The heart is a mechanical system with muscles pumping and valves opening and shutting, and it sends out a signature of sounds and motions, which an EKG does not detect. EKGs also say nothing about lung function,” said Farrokh Ayazi, Ken Byers Professor in Georgia Tech’s School of Electrical and Computer Engineering.
Stethoscope-accelerometer combo
The chip, which acts as an advanced electronic stethoscope and accelerometer in one, is aptly called an accelerometer contact microphone. It detects vibrations that enter the chip from inside the body while keeping out distracting noise from outside the body's core like airborne sounds
“If it rubs on my skin or shirt, it doesn’t hear the friction, but the device is very sensitive to sounds coming at it from inside the body, so it picks up useful vibrations even through clothing,” Ayazi said.
The detection bandwidth is enormous - from broad, sweeping motions to inaudibly high-pitched tones. Thus, the sensor chip records all at once fine details of the heartbeat, waves the heart sends through the body, and respiration rates and lung sounds. It even tracks the wearer’s physical activities such as walking.
The signals are recorded in sync, potentially offering the big picture of a patient’s heart and lung health. For the study, the researchers successfully recorded a “gallop,” a faint third sound after the “lub-dub” of the heartbeat. Gallops are normally elusive clues of heart failure.
The researchers published their results in the journal npj Digital Medicine on February 12, 2020. The research was funded by the Georgia Research Alliance, the Defense Advanced Research Projects Agency (DARPA), the National Science Foundation, and the National Institutes of Health. Study coauthor Divya Gupta, M.D., a cardiologist at Emory University, collaborated in testing the chip on human participants.
Hermetically sealed vacuum
Medical research has tried to make better use of the body’s mechanical signals for decades but recording some – like waves traversing multiple tissues – has proven inconsistent, while others – like gallops – have relied upon clinician skills influenced by human error. The new chip produces high-resolution, quantified data that future research could match to pathologies in order to identify them.
“We are working already to collect significantly more data matched with pathologies. We envision algorithms in the future that may enable a broad array of clinical readings,” Ayazi said.
Though the chip’s main engineering principle is simple, making it work and then manufacturable took Ayazi’s lab ten years, mainly because of the Lilliputian scale of the gap between the silicon layers, i.e. electrodes. If the 2-millimeter by 2-millimeter sensor chip were expanded to the size of a football field, that air gap would be about an inch wide.
“That very thin gap separating the two electrodes cannot have any contact, not even by forces in the air in between the layers, so the whole sensor is hermetically sealed inside a vacuum cavity,” Ayazi said. “This makes for that ultralow signal noise and breadth of bandwidth that are unique.”
Detects through clothing
The researchers used a manufacturing process developed in Ayazi’s lab called the HARPSS+ platform (High Aspect Ratio Poly and Single Crystalline Silicon) for mass production, running off hand-sized sheets that were then cut into the tiny sensor chips. HARPSS+ is the first reported mass manufacturing process that achieves such consistently thin gaps, and it has enabled high-throughput manufacturing of many such advanced MEMS, or microelectromechanical systems.
The experimental device is currently battery-powered and uses a second chip called a signal-conditioning circuit to translate the sensor chip’s signals into patterned read-outs.
Three sensors or more could be inserted into a chest band that would triangulate health signals to locate their sources. Someday a device may pinpoint an emerging heart valve flaw by turbulence it produces in the bloodstream or identify a cancerous lesion by faint crackling sounds in a lung.
Here's how to subscribe to our free science and technology newsletter
Also read: Digital tool helps with tough COVID19 decision
These researchers co-authored the study: Pranav Gupta (first author), Mohammad Moghimi, Yaesuk Jeong and Omer Inan from Georgia Tech. The research was funded by the Georgia Research Alliance, the Defense Advanced Research Projects Agency (DARPA) Technology Office’s Advanced Inertial Micro Sensors program (contract # N66001-16-1-4064), and by the National Science Foundation/National Institutes of Health Smart and Connected Health Program (grant # R01 EB023808). The team’s work with human subjects was approved by Emory University and Georgia Institute of Technology Institutional Review Boards (IRB# H18248). Any findings, conclusions or recommendations are those of the authors and not necessarily of the sponsors.
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Apr. 13, 2020
What-if questions can torment a doctor making coronavirus retest decisions: What if a patient’s initial negative test was a false negative, and he or she needs a second test? What if they don’t need it, and a retest would use up a scarce test kit and treatments that other patients need?
Such challenges led Piedmont Healthcare in Atlanta to establish a paper-based decision tree for ordering COVID-19 retests, and researchers at the Georgia Institute of Technology turned it into an automated digital tool. Piedmont further developed the tool and has now built it into the hospital’s electronic medical record, where it influences the ordering of retests.
A user can answer their “ifs” by clicking through questions, and the “if-this-then-do-that” algorithm makes recommendations for best courses of action, ranging from immediately treating a patient for COVID-19 to retesting to consulting a specialist. The final decision remains with the physician.
The questions are deceptively simple, but the recommendations are not always obvious. That reflects the algorithm’s usefulness to fill gaps in thinking about the new sickness, which can confront clinicians with surprises.
“If a patient has not had close contact with positive patients and the first test came back negative, a physician may think the patient does not need to be retested. But actually, the patient may need a second test because they are in intensive care and also have suspicious chest X-rays,” said Georgia Tech graduate research assistant April Yu, who converted the decision tree into a digital tool.
“One of our big worries in using a brand-new test like the coronavirus test is that it will miss real cases, and this tool helps prevent that,” said Dr. Bronwen Garner, who helped develop the original decision tree and is an infectious disease specialist at Piedmont Healthcare. “It also helps reassure physicians when they get a negative result that it is probably a true negative.”
Suspenseful decision-making
A physician’s reaction to an initial negative test can mean life or death because the physician not only decides on follow-up testing but also on treatment pathways and quarantine.
“If you make a misstep in the thought process, it can lead to cascading impacts not only for the patient but also for healthcare professionals and family members, who may be exposed to the patient,” said Pinar Keskinocak, William W. George Chair and Professor in Georgia Tech’s Stewart School of Industrial and Systems Engineering. “This tool is meant to help doctors easily stay on the decision tree path.”
Michael O’Toole, executive director of Piedmont Healthcare’s quality improvement department, originally pictured doctors getting an automated version of the decision tree to use on their phones. O’Toole called Keskinocak, and she tapped Yu, a member of her research group.
“Literally within four hours they had it ready for us. It was incredible,” said O’Toole, a Georgia Tech alumnus who studied industrial and systems engineering.
“It was a very pleasant surprise,” said Dr. Garner, who is also a Georgia Tech graduate. “Automated tools are better than a paper format because they’re in the same format as orders in our electronic system. We get notifications in real time instead of having to remember to check a piece of paper.”
The tool is in place in the system where doctors order retests and is specific to Piedmont’s workflow. It may not be directly transferable to other health care systems.
Piedmont Healthcare simplified the logic even more, and the hospital built its own custom alerts to guide physicians on retesting. For cases that are more ambiguous, Piedmont Healthcare’s final version of the tool also gives physicians inside the hospital guidance to consult with their in-house infectious disease specialists.
If-this-then-retest
In her original version, Yu had turned the decision tree criteria into a short panel of questions with yes and no answers. It took her six iterations to arrive at her final version.
Yu’s version asked whether the patient:
- has a relevant ailment
- previously tested positive for coronavirus
- is now in an intensive care unit
- has worsening lung conditions
- shows telltale lung damage in imaging
- has been diagnosed with a different ailment
- the patient has had contact with someone else who tested positive for coronavirus.
On the back end, the algorithm guided the user through risks of coronavirus presence based on the answers.
“The steps were easy to follow, and the answers were color-coded for urgency with white, yellow, and red,” said Keskinocak, who also directs Georgia Tech’s Center for Health and Humanitarian Systems.
One bright yellow answer read: “This patient needs re-testing 24 hours after the initial test!” And there were further recommendations on how to handle the case.
Here's how to subscribe to our free science and technology newsletter
Also read: Advice on DIY masks
Writer & Media Representative: Ben Brumfield (404-272-2780), email: ben.brumfield@comm.gatech.edu
Georgia Institute of Technology
Feb. 11, 2020
Four Georgia Institute of Technology faculty members have been elected as new members of the National Academy of Engineering (NAE). Marilyn Brown, Thomas Kurfess, Susan Margulies, and Alexander Shapiro join 83 other new NAE members for 2020 when they are formally inducted during a ceremony at the academy’s annual meeting on Oct. 4 in Washington, D.C.
Election of new NAE members, the culmination of a yearlong process, recognizes individuals who have made outstanding contributions to "engineering research, practice, or education, including, where appropriate, significant contributions to the engineering literature" and to "the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education."
“It’s the honor of a lifetime to be recognized by the National Academy of Engineering for the impact we’ve have on understanding lung injuries in the critical care unit and traumatic brain injuries in children,” said Margulies, chair of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University and, with Brown, one of just three women on the Georgia Tech faculty accorded NAE membership – one of the highest professional distinctions an engineer can receive.
“Our work is deeply collaborative, and I am grateful to the engineers, scientists, physicians, and patients who are partners in our journey,” Margulies added.
Margulies, a researcher in the Petit Institute for Bioengineering and Bioscience at Tech and a Georgia Research Alliance Eminent Scholar in Injury Biomechanics at Emory, was elected, “for elaborating the traumatic injury thresholds of brain and lung in terms of structure-function mechanisms,” according to the NAE announcement.
Using an integrated biomechanics approach, Margulies’ research program spans the micro-to-macro scales in two distinct areas, traumatic brain injury and ventilator-induced lung injury. Her work has generated new knowledge about the structural and functional responses of the brain and lungs to their mechanical environment. Margulies came to Georgia Tech in 2017 from the University of Pennsylvania, where she’d been a professor of bioengineering, and had earned her Master of Science in Engineering and Ph.D. in Bioengineering.
Brown, a Regents and Brook Byers Professor of Sustainable Systems in the School of Public Policy, was co-recipient of the Nobel Peace Prize in 2007 (for co-authorship of the Intergovernmental Panel on Climate Change Working Group III Assessment Report on Mitigation of Climate Change, Chapter 6).
She joined Georgia Tech in 2006 after a career at the U.S. Department of Energy's Oak Ridge National Laboratory, where she led several national climate change mitigation studies and became a leader in the analysis and interpretation of energy futures in the United States. Her research at Tech focuses on the design and impact of policies aimed at accelerating the development and deployment of sustainable energy technologies, emphasizing the electric utility industry. She was elected to NAE “for bridging engineering, social and behavioral sciences, and policy studies to achieve cleaner electric energy.”
Brown, who earned her Ph.D. at the Ohio State University, co-founded and chaired the Southeast Energy Efficiency Alliance, served two terms as a presidential appointee on the board of the Tennessee Valley Authority – the nation’s largest public power provider – and also served two terms on the U.S. Department of Energy’s Electricity Advisory Committee, where she led the Smart Grid Subcommittee.
“The most rewarding feature of my career has been working toward solutions with colleagues across disciplines,” Brown said.
Shapiro is the Russell Chandler III Chair and professor in the H. Milton Stewart School of Industrial and Systems Engineering, where his research is focused on stochastic programming, risk analysis, simulation-based optimization, and multivariate statistical analysis.
In 2013, he was awarded the INFORMS Khachiyan Prize for lifetime achievements in optimization. He received the 2018 Dantzig Prize from the Mathematical Optimization Society and the Society for Industrial and Applied Mathematics.
Since earning his Ph.D. in applied mathematics-statistics from Israel’s Ben-Gurion University of the Negev in 1981, Shapiro has made substantial contributions to the fields of optimization and large-scale, stochastic programming, and he was elected to NAE “for contributions to the theory, computation, and application of stochastic programming.”
Kurfess is professor and HUSCO/Ramirez Distinguished Chair in Fluid Power and Motion Control in the George W. Woodruff School of Mechanical Engineering, where he has helped guide the evolution of technology as a pioneer in the digital transformation of manufacturing.
Improving manufacturing technology is a pursuit that has roots in his childhood. “I grew up in my father’s machine shop,” said Kurfess, who has a special fondness for mom-and-pop operations. He was elected by the NAE “for development and implementation of innovative digital manufacturing technologies and system architectures.”
“I’m proud that the work we do has a positive impact on small and medium-sized enterprises, which are about 99% of the manufacturing operations, as well as large operations,” said Kurfess, who earned all of his degrees at MIT. “Our work targets people who are implementing the digital thread in manufacturing, and what the digital thread will do is make sure those smaller enterprises, those mom and pops, can have access to the latest and greatest technologies.”
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contact: John Toon (404-894-6986) (jtoon@gatech.edu).
Writer: Jerry Grillo
News Contact
John Toon
Research News
(404) 894-6986
Pagination
- Previous page
- 5 Page 5