Feb. 21, 2021
The President's Undergraduate Research Award pays selected students $1500 to conduct undergraduate research. Applications for summer 2021 funding are due on February 26, 2021.
Apply online at urop.gatech.edu
Nov. 30, 2020
When one or more coronavirus vaccines receives FDA emergency use authorization, it will launch a public health and logistics initiative unlike any in U.S. history.
Hundreds of millions of doses will have to distributed nationwide and kept cold until healthcare professionals can administer not one, but two doses to each person. And enough skeptical members of the population will have to be persuaded to receive the vaccine to slow virus transmission.
Beyond those challenges, the distribution effort will have to adapt to unexpected and uneven demand; accommodate recipients who may not return on time for a second dose; train hundreds of thousands of staff from clinics, pharmacies, doctor’s offices, and hospitals; prioritize serving high-risk groups first while encouraging others to wait — all while under tremendous pressure to get the much-anticipated vaccines into use as case counts and the death toll continue rising.
“Time is of the essence because the virus is already so widespread,” said Pinar Keskinocak, the William W. George Chair and professor in the H. Milton Stewart School of Industrial and Systems Engineering (ISyE) and director of the Center for Health and Humanitarian Systems at the Georgia Institute of Technology. “With the pressure on our timeline, knowledge of how quickly the disease is spreading, and the broad U.S. and global need, I can’t think of a comparable public health initiative that has ever been undertaken.”
Shipping and Keeping Hundreds of Millions of Doses Cold
Three vaccines, produced by Moderna, Pfizer and its German partner BioNTech, and Oxford-AstraZeneca, are expected to be available first. The Pfizer-BioNTech vaccine will need to be kept ultra-cold — minus 94 degrees Fahrenheit — on its journey to individual Americans. The Moderna drug won’t have such demanding conditions, but both it and the Pfizer vaccine will tax the existing “cold chain” that keeps vaccines and other temperature-sensitive products in a narrow range of conditions during transport and storage.
The Oxford-AstraZeneca vaccine will have much less stringent requirements and faster ramp-up in capacity, though early testing suggests its efficacy may be lower than the others. That will create tradeoffs between efficacy versus access and speed in distribution.
Plans already exist to get the vaccines from manufacturers to the states, each of which has developed its own distribution plan. Keskinocak worries mostly about “last mile” plans — getting the vaccines to where they will be injected — and getting individuals to those locations.
“Access is going to be a challenge,” she said. “You may be able to get it to locations where it can be distributed, but you have to make sure the people who really need the vaccine can easily access those locations.”
Cold chain transportation, tracking, tracing, and storage already exist in most areas, but refrigeration could be challenging for rural areas that may be at the end of the chain, especially for the vaccine requiring very cold temperatures beyond the capability of freezers found in most doctor’s offices and clinics. And cold can sometimes be too cold, Keskinocak said.
“We often think about keeping it cold, but sometimes it may be too cold, which is not good. It’s not just whether the temperature exceeded the required level, but also whether it went below that. It is important to keep the vaccine exactly at the required temperature level.”
Pfizer has developed a shipping container that includes a temperature tracking device — and 50 pounds of dry ice to maintain the right temperature during transit. Because it is contained in small vials and the liquid vaccine is diluted for use, the overall volume being shipped will be relatively small, limiting the number of packages that will be moved and stored, Keskinocak noted.
Ultimately, the cold chain may play a significant role in vaccine effectiveness. Currently, the vaccines being produced by Pfizer/BioNTech and Moderna are reported to have a higher efficacy than the Oxford-AstraZeneca vaccine — but only if they can be maintained at the proper temperatures. The timing, magnitude, and duration of temperature fluctuations during transport and before administration could affect that in ways that may be difficult to assess.
“Our current modeling shows that a vaccine that is less effective but that can be distributed more quickly and more widely might work better in some settings than a more effective vaccine, thereby reducing the total number of infections in the population,” Keskinocak said.
If You Build It, Will They Come?
Expectations are that the nation is hungry for a vaccine to escape the horrors of Covid-19. But a recent Gallup survey shows that only 58% of respondents said they planned to receive the vaccine when it becomes available. Boosting that percentage will require a massive communications effort to overcome vaccine reluctance and concerns fueled by the uneven nature of the U.S. pandemic response.
“If we can get the vaccine to locations where people can access it, and we have the necessary syringes, supplies, and PPE, as well as the healthcare staff to administer the injections, it’s not clear that people will come to receive it in large enough numbers,” Keskinocak said. “That’s one major component missing from a lot of the plans that I see at the state level.”
The communications program will have to run in parallel to the vaccine distribution, and they have to be coordinated so that supply meets demand.
“Public health communication and dissemination of information at the right time and in the right language is going to be at least as important and challenging as the logistics of distributing the vaccine,” Keskinocak said. “Communication is going to shape demand to a large extent. If one is more effective than the other, we will have a mismatch between demand and supply.”
Different demographic populations have different levels of trust for medicine in general and vaccines in particular, she said, so communications campaigns will have to focus on issues of concern to those groups. Unexpected variations in vaccine demand caused by these concerns could also create logistical uncertainties.
“We can try to forecast demand, and ship supplies to those locations,” she said. “But historically, we have seen that demand can exceed supply in one location while inventory builds up in another location. We need to avoid this situation of unmet demand and unused vaccine.”
Another issue will be the two doses necessary for the vaccine. The second dose must be received within a narrow range of time for the two-dose vaccine to be effective. Should a second dose be reserved for every person receiving a first dose, or should the goal be to get as many doses out as possible?
“Some people may never show up to be vaccinated, while others will receive the first dose, but may not come back for the second dose,” she said.
Getting the Program Started
The first available doses will likely go to healthcare workers and first responders who are on the front lines of battling Covid-19. That is expected to be the easier part of vaccination logistics, and the lessons learned there should help with the much more massive vaccination campaign for high-risk individuals and the general public.
As vaccine production and distribution capacity ramp up, other groups will be next in line. While distributing small batches as manufacturers produce it can create some supply challenges, that also allows the system to more easily adjust to unexpected demand.
Even though distributing and administering vaccines is something the U.S. healthcare system does routinely, the size and timeline of this project are unprecedented, Keskinocak noted.
Beyond the logistical and communications needs, the vaccination program will also have a strong information technology component. Administration will likely be by appointment, and each injection will have to be reported to a vaccine registry to provide a record of which vaccines people have received and when.
Vaccinating People Who May Already Be Immune
It’s estimated that the number of reported Covid-19 cases may be just 10% of the actual number of infections in the U.S. Assuming recovery from the virus confers immunity for some period of time means there may be quite a few people who don’t actually need the vaccine right away to be protected. But there are currently no plans to determine whether recipients are already immune before they receive the vaccine.
“There are a lot of people out there who have some level of immunity to the coronavirus,” Keskinocak said. “The plans I’ve seen don’t include the serological testing that would be needed to identify people with some level of immunity, which could be around 30% of the population by the time the vaccine gets out to the general public.”
Testing for immune antibodies could be done ahead of the vaccination program, but that would create an extra step in a process that is already quite complicated. Healthcare systems such as the U.S. Department of Veterans Affairs or certain private insurance plans could include that step, especially if vaccine supplies lag behind demand.
“The big complexity is timing,” she said. “Once vaccines become available, you’ll want to deliver them as quickly as possible to as many people as possible in a very short time frame.”
Annual vaccination campaigns for the seasonal flu set ambitious goals for the population levels they want to reach, but the time challenges will be much greater for the coronavirus vaccine.
“The seasonal flu vaccine becomes available months before the virus spreads broadly, so we have quite a bit of time to administer it before we get into the peak of the flu season,” she said. “We have been in the midst of the Covid-19 pandemic for several months now. We are really late in the game, so we don’t have the luxury of time.”
Keskinocak is cautiously optimistic that the challenges will ultimately be addressed.
“There are certainly still lots of unknowns,” she said. “But the state plans I have seen look reasonable from a supply chain standpoint. Some of the decisions will be made once the states receive the vaccine, and exactly how they do it will be somewhat up to the local jurisdictions. There are still many things that need to be decided to make this unprecedented initiative live up to its goals.”
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contact: John Toon (404-894-6986) (jtoon@gatech.edu)
Writer: John Toon
News Contact
John Toon
Research News
(404-894-6986)
Nov. 18, 2020
Georgia Institute of Technology is a governing member of the BioIndustrial Manufacturing and Design Ecosystem (BioMADE), a nonprofit that recently won a seven-year, $87 million award from the U.S. Department of Defense (DoD).
Created by the Engineering Biology Research Consortium, BioMADE will collaborate with public and private entities to advance sustainable and reliable bioindustrial manufacturing technologies. Headquartered at the University of Minnesota in St. Paul, BioMADE includes some of the largest bioindustrial manufacturing employers in the U.S. working in conjunction with some of the top educators in the world.
In support of this collaboration, the $87 million in DoD funding will be combined with more than $187 million in non-federal cost-share from 31 companies, 57 colleges and universities, six nonprofits, and two venture capital groups across 31 states.
Pamela Peralta-Yahya, an associate professor in Georgia Tech’s School of Chemistry and Biochemistry and School of Chemical and Biomolecular Engineering, is Tech’s representative to BioMADE’s Leadership Council, which will set the organization’s funding priorities.
Peralta-Yahya says, “An incredible cross section of Georgia Tech faculty contributed to the BioMADE proposal; over 30 faculty members, spanning five Schools across the College of Science, College of Engineering, and the Ivan Allen College of Liberal Arts.”
She notes: “Georgia Tech’s involvement in BioMADE is poised to catalyze interdisciplinary collaborations across the university, from data science and downstream processing to supply chain logistics and the policy, legal, and biosafety implications of bioindustrial applications. The projects funded by BioMADE will give undergraduates and graduate students a springboard to the emerging biomanufacturing and related areas.”
Mark Styczynski, an associate professor in Georgia Tech’s School of Chemical and Biomolecular who is Tech’s representative to the BioMADE Technical Committee, says: “Georgia Tech will be a member of BioMADE at the governing level, the highest level of engagement for academic institutions. We are excited about the resulting opportunities for Georgia Tech to bring to bear its manufacturing, chemical, and biochemical expertise on new applications and focus areas in the biomanufacturing space.”
He adds: “Our involvement in this area is a great complement to other biomanufacturing efforts at Georgia Tech and will contribute to a rapidly growing bioeconomy in Georgia.”
Through a close relationship with DoD and the Military Services, BioMADE will work to establish long-term and dependable bioindustrial manufacturing capabilities for a wide array of products. Anticipated bioindustrial manufacturing applications include the following products: chemicals, solvents, detergents, reagents, plastics, electronic films, fabrics, polymers, agricultural products (e.g. feedstock), crop protection solutions, food additives, fragrances, and flavors.
BioMADE’s efforts will examine and advance industry-wide standards, tools, and measurements; mature foundational technologies; foster a resilient bioindustrial manufacturing ecosystem; advance education and workforce development; and support the establishment and growth of supply chain intermediaries that are essential for a robust U.S. bioeconomy. Other important focus areas include challenges related to biosafety and security and ethical, legal, and societal considerations.
Stefan France, an associate professor in Georgia Tech’s School of Chemistry and Biochemistry is Tech’s representative to BioMADE’s Education and Workforce Committee, which will help craft and implement the organization’s strategic plan.
France explains that this committee “will concentrate its efforts in three major areas: curriculum and training for the bioindustrial workforce, promoting awareness of career opportunities, and coordination across the STEM community, the biomanufacturing ecosystem, and the training pipeline—everything from K-12 to community and technical colleges to four-year colleges, graduate programs, and post-graduate training.”
News Contact
Brad Dixon, braddixon@gatech.edu
Oct. 07, 2020
California, September 14, 2020: TiE Global hosted the 2nd edition of the TiE University Pitch Competition over the weekend. Cash prizes of close to $14,000 and almost $35,000 worth of in-kind prizes were given out to the 13 participants. TiE Atlanta’s Aerodyme Technologies from Georgia Institute of Technology came in first, winning $5000. TiE Silicon Valley’s team Ambii from San Jose State University bagged the second prize, winning $3000; while TiE Toronto’s LSK Technologies, a MedTech startup from the University of Toronto emerged as the third winner, winning $2000.
The winning team, Aerodyme Technologies has created a novel device that saves fuel costs for tractor-trailers by minimizing aerodynamic drag. Ambii, which came in second, provides an in-store music streaming platform for retail outlets, cafes and restaurants without the hassles of licensing. Third prize winner, LSK Technologies, created a diagnostic device for testing infectious diseases such as Covid19 at the point of need.
Congratulating the winning team, Mahavir Pratap Sharma, Chairman of the TiE Global Board of Trustees said, "We are proud of these young talented entrepreneurs. Their growth story from pitches at their local TiE Chapters till the Global Finals has seen a massive expansion and iteration of thought and structure. This is a complete team effort put forward by the program co-chairs and charter member mentors who helped them grow their idea, giving them thorough guidance and mentoring the students over the last few months to compete on a global stage.”
Aerodyme Technologies participated in Georgia Tech’s CREATE-X Startup Launch program during summer 2019. During the startup accelerator program, the Aerodyme team was able to conduct customer discovery and receive mentorship and funding to take their product to market. The team also won 2nd place in the 12th annual InVenture Prize competition in March 2020. As part of the competition, Aerodyme received $10,000 in cash and patent filing assistance funded by the Georgia Tech Research Corporations.
The second edition of the TiE University jointly organized by TiE Atlanta & TiE Hyderabad had 13 teams representing TiE chapters from India, Israel, UAE, Israel, USA, and Canada. These teams were previously the chapter winners and were then mentored to participate in the Global finals. After the Semi-final round on Saturday, seven teams were selected for the finals. Teams had a 10-minute pitch to an eminent Jury panel and a 5-minute live Q&A.
Speaking at the Presentation Ceremony the TiE University program co-chairs Dr. Paul Lopez, SubbaRaju Pericherlaand Viiveck Verma, said they are looking to expand the program participation to 40 chapters and 400+ universities worldwide by 2022.
The worldwide jury panel for the finals, consisting of VCs and investors, included Bodhi Capital’s Dharti Desai, Silicon Valley Bank’s Priya Rajan, Elevate Capital’s Kumar Sripadam, and Inflexor Ventures’ Venkat Vallabhaneni. Semi-finals judges from across the globe included Craig Abbott, Rakesh Bhatia, Radhika Iyengar, Rama Devi Kanneganti, Doc Parghi, and Sonia Weymuller.
Apart from the top three winners, prizes were announced in various other categories. Silicon Valley’s Ambii and New Jersey’s Volant from New Jersey Institute of Technology jointly received a $1,500 Best Elevator Pitch award. Similarly, Teams Clean Electric from IIT/BHU, Varanasi representing TiE Mumbai, and Aruga Technologies from Carnegie Mellon University representing TiE Pittsburgh jointly received $1,500 Best Technology prize. Frinks, from IIT Hyderabad, representing TiE Hyderabad took the $500 People's Choice Award. Apart from this, all participating teams walked away with technology and service prizes worth $2500 per team.
The competition also hosted a keynote address by serial entrepreneur Thejo Kote. Thejo sold his connectivity startup, Automatic for $115 million to SiriusXm. He inspired the university startup teams and online audience alike by saying, “The biggest lesson I’ve learned along the way is to make sure you enjoy the journey (of building a startup) and it’s something that you learn from and grow from. Else it will be a lot more challenging.”
About TiE University:
TiE University program focuses on enhancing the learning objectives of university students globally through the creation and presentation of business pitches for startups and new small business ventures so that they aspire to become entrepreneurs. TiE University is looking to expand its reach to 40 chapters and 400+ universities worldwide. If you’re interested, reach out to the below-mentioned media contact. For more information, visit - https://tie.org/tie-university/
About TiE Global:
TiE Global, is a non-profit organization dedicated to fostering entrepreneurship around the World. TiE strives to inspire entrepreneurs through mentoring, networking, education, incubating and funding programs and activities. With nearly 2000+ events held each year, TiE brings together the entrepreneurial community to learn from local leaders, as well as each other. Few of the annual flagship events conducted by TiE are TYE, TiE Women, TiE University, TiECons and TGS. For more information, please visit our website at https://tie.org/
Media Contact:
Aparna Mishra Aparna@tie.org
Oct. 07, 2020
By Jessica Barber
On Wednesday, September 16, the Office of Undergraduate Education (OUE) hosted the kick-off session for the 13th Annual InVenture Prize. With over $35,000 in prizes, the competition is the holy grail of college entrepreneurship. Although the InVenture Prize officially starts in January 2021, students have already begun their preparations and idea declarations.
Unlike previous years, the kick-off was hosted online through Gatherly, a virtual event platform recently built by none other than Georgia Tech students. Despite this, attendees did not miss a beat. The kick-off marked a return to normalcy for the Georgia Tech innovation community from learning key information about the competition to directly speaking with past winners.
After a welcome from interim Assistant Director of Student Innovation, Recha Reid, students were given an overview of some upcoming InVenture Prize events, including the ongoing Pitch Your Idea and IdeaBuzz sessions. Students were given an overview of OUE’s customer discovery, financial forecasting, marketing, and patent/copyright workshops. From there, the floor was turned over to Dr. Chris Reaves, executive director of the office for Academic Enrichment Programs.
“At its core, the InVenture Prize is an invention startup competition, but we work together — even the teams work with each other — to help one another. We achieve more, grow more, and develop our companies better when we’re helping each other, and that’s a big part of what we’re doing,” Reaves explained.
Later, students were given the opportunity to speak with representatives from Queues and Aerodyme, the respective first- and second-place winners of the 2020 InVenture Prize. Students learned firsthand what it takes to succeed on the InVenture Prize stage; the teams later offered advice on the invention process, their lessons learned, and the visibility benefits of participating in the competition.
“If you’re on the edge right now about doing InVenture Prize, definitely do it. We actually had that same thought before we did it, and we’re just so glad that we did. It’s a lot of work, and you’re going to step outside of your comfort zone, but it’s so worth it”, said Joy Bullington of team Aerodyme Technologies.
Queues team member Sam Porta similarly had some words of encouragement for those looking into the 2021 InVenture Prize.
“The difference between an entrepreneur and someone who’s just engineering something is persistence, and the InVenture Prize is a great opportunity to test this. If you think you’ve come up with something great that has a lot of value, then, by all means, do it,” Porta emphasized.
Towards the end of the session, students were invited to visit virtual “booths” dedicated to areas of health, retail, fintech, transportation, education tools, gaming, and networking.
“InVenture is honestly one of the reasons I chose to come to Tech, and I’m just so excited to come into with something that I’m really confident about,” an attendee said.
“The most interesting thing about tonight was hearing from the past winners and having them talk about their experiences. Definitely super excited to apply, and hopefully we do really well,” another stated.
Registration for the 2021 InVenture Prize will remain open until January. Student innovators are invited to check out OUE’s information and development sessions to be held throughout the Fall semester. All dates and related topics can be found at innovation.gatech.edu and inventureprize.gatech.edu.
FIND OUT MORE ABOUT THE 2021 INVENTURE PRIZE BY CLICKING HERE
Visit us on
Instagram @gtinventure
Twitter @InVenturePrize
Sep. 04, 2020
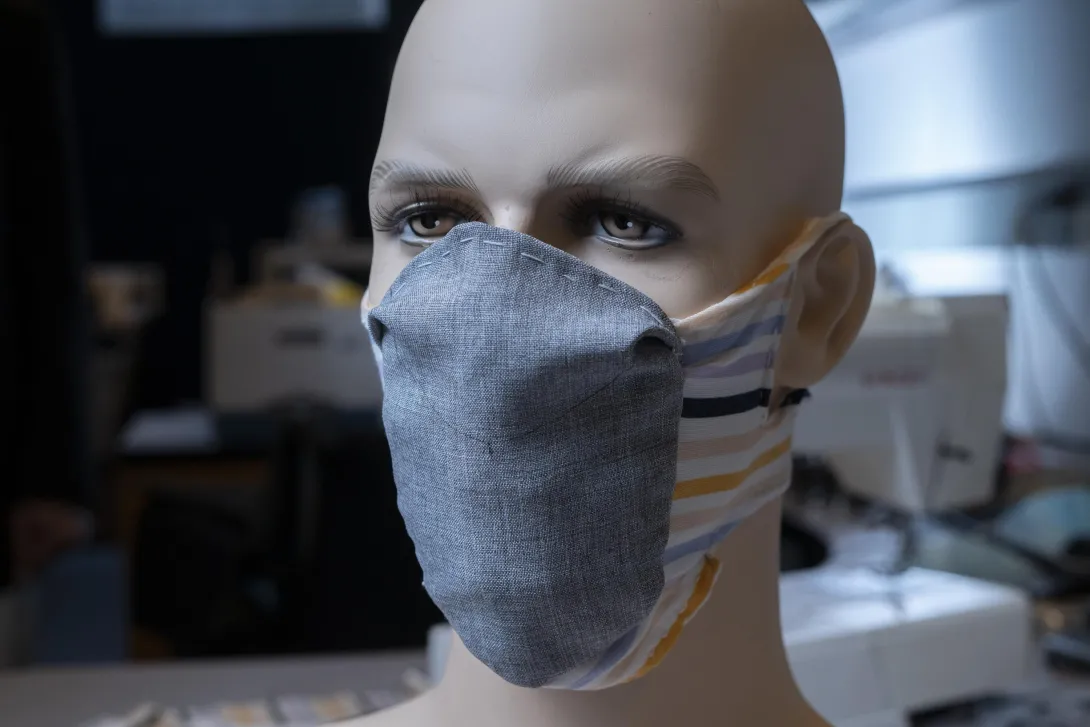
Imagine a reusable face mask that protects wearers and those around them from SARS-CoV-2, is comfortable enough to wear all day, and stays in place without frequent adjustment. Based on decades of experience with filtration and textile materials, Georgia Institute of Technology researchers have designed a new mask intended to do just that — and are providing the plans so individuals and manufacturers can make it.
The modular Georgia Tech mask combines a barrier filtration material with a stretchable fabric to hold it in place. Prototypes made for testing use hook and eye fasteners on the back of the head to keep the masks on, and include a pocket for an optional filter to increase protection. After 20 washings, the prototypes have not shrunk or lost their shape.
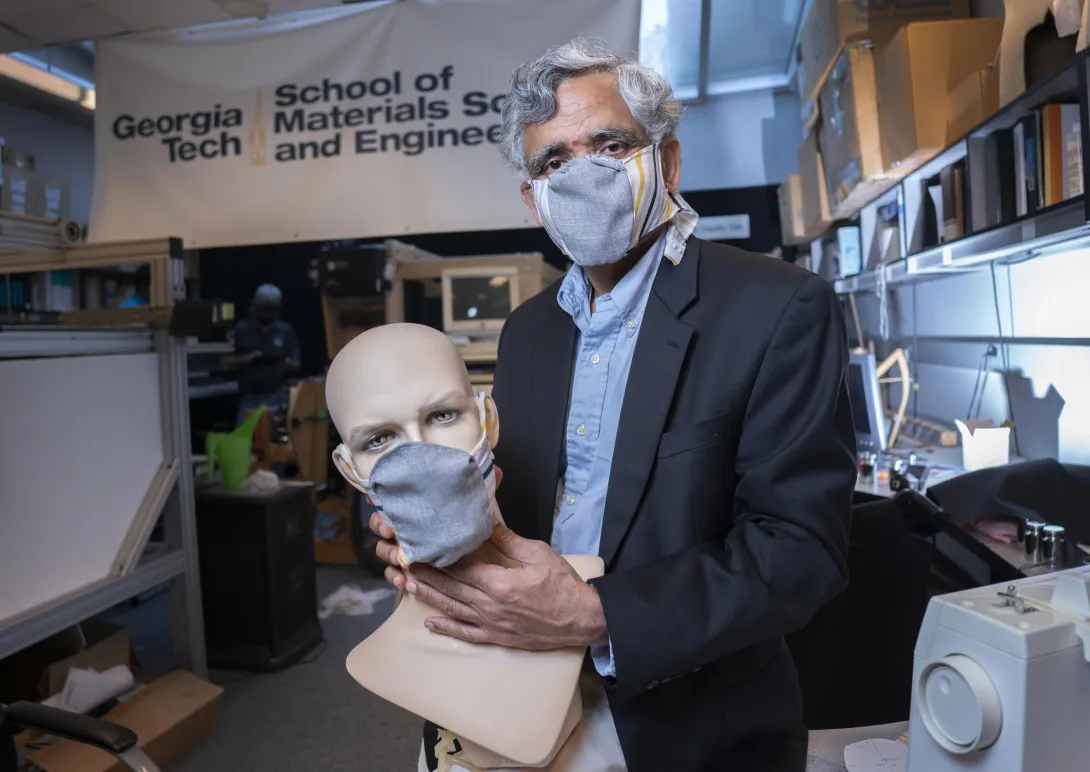
“If we want to reopen the economy and ask people to go back to work, we need a mask that is both comfortable and effective,” said Sundaresan Jayaraman, the Kolon Professor in Georgia Tech’s School of Materials Science and Engineering. “We have taken a science-based approach to designing a better mask, and we are very passionate about getting this out so people can use it to help protect themselves and others from harm.”
The fundamental flaw in existing reusable cloth masks is that they — unlike N95 respirators, which are fitted for individual users — leak air around the edges, bypassing their filtration mechanism. That potentially allows virus particles, both large droplets and smaller aerosols, to enter the air breathed in by users, and allows particles from infected persons to exit the mask.
The leakage problem shows up in complaints about eyeglasses fogging up as exhaled breath leaks around the nose, making people less likely to wear them. The fit problem can also be seen in constant adjustments made by wearers, who could potentially contaminate themselves whenever they touch the masks after touching other surfaces.
To address the leakage challenge, Jayaraman and principal research scientist Sungmee Park created a two-part mask that fastens behind the head like many N95 respirators. The front part — the barrier component — contains the filtration material and is contoured to fit tightly while allowing space ahead of the nose and mouth to avoid breathing restrictions and permit unrestricted speech. Made from the kind of moisture-wicking material used in athletic clothing, it includes a pocket into which a filter can be inserted to increase the filtration efficiency and thereby increase protection. The washable fabric filter is made of a blend of Spandex and polyester.
The second part of the mask is fashioned from stretchable material. The stretchable part, which has holes for the ears to help position the mask, holds the front portion in place and fastens with conventional hook and eyelet hardware, a mechanism that has been used in clothing for centuries.
“We want people to be able to get the mask in the right place every time,” Jayaraman said. “If you don’t position it correctly and easily, you are going to have to keep fiddling with it. We see that all the time on television with people adjusting their masks and letting them drop below their noses.”
Beyond controlling air leakage, designing a better mask involves a tradeoff between filtration effectiveness and how well users can breathe. If a mask makes breathing too difficult, users will simply not use it, reducing compliance with masking requirements.
Many existing mask designs attempt to increase filtration effectiveness by boosting the number of layers, but that may not be as helpful as it might seem, Park said. “We tested 16 layers of handkerchief material, and as we increased the layers, we measured increased breathing resistance,” she said. “While the breathing resistance went up, the filtration did not improve as much as we would have expected.”
“Good filtration efficiency is not enough by itself,” said Jayaraman. “The combination of fit, filtration efficiency, and staying in the right place make for a good mask.”
The stretchable part of the mask is made from knitted fabric — a Spandex/Lyocell blend — to allow for stretching around the head and under the chin. The researchers used a woven elastic band sewn with pleats to cover the top of the nose.
The researchers made their mask prototypes from synthetic materials instead of cotton. Though cotton is a natural material, it absorbs moisture and holds it on the face, reducing breathability, and potentially creating a “petri dish” for the growth of microbes.
“Masks have become an essential accessory in our wardrobe and add a social dimension to how we feel about wearing them,” Park said. So, the materials chosen for the mask come in a variety of colors and designs. “Integrating form and function is key to having a mask that protects individuals while making them look good and feel less self-conscious,” Jayaraman said.
The work of Jayaraman and Park didn’t begin with the Covid-19 pandemic. They received funding 10 years ago from the Centers for Disease Control and Prevention to study face masks during the avian influenza outbreak. Since then Jayaraman has been part of several National Academy of Medicine initiatives to develop recommendations for improved respiratory protection.
Covid-19 dramatically increased the importance of using face masks because of the role played by asymptomatic and pre-symptomatic exposure from persons who don’t know they are infected, Jayaraman said. While the proportion of aerosol contributions to transmission is still under study, they likely increase the importance of formfitting masks that don’t leak.
Jayaraman and Park have published their recommendations in The Journal of The Textile Institute, and will make the specifications and patterns for their mask available to individuals and manufacturers. The necessary materials can be obtained from retail fabric stores, and the instructions describe how to measure for customizing the masks.
“There is so much misinformation about what face masks can do and cannot do,” Jayaraman said. “Being scientists and engineers, we want to put out information backed by science that can help our community reduce the harm from SARS-CoV-2.”
Link to plans, patterns and specifications for this mask
CITATION: Sungmee Park and Sundaresan Jayaraman, “From containment to harm reduction from SARS-CoV-2: a fabric mask for enhanced effectiveness, comfort, and compliance.” (The Journal of The Textile Institute, 2020) https://doi.org/10.1080/00405000.2020.1805971
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Contact: John Toon (404-894-6986) (jtoon@gatech.edu).
Writer: John Toon
News Contact
John Toon
Research News
(404) 894-6986
Aug. 06, 2020
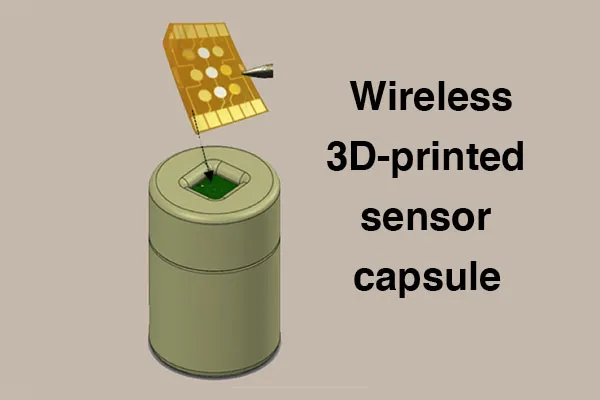
BioFabUSA, a Department of Defense-funded Manufacturing Innovation Institute within the Manufacturing USA network, has awarded the Georgia Institute of Technology and industry partner Rockwell Automation a project entitled, “Wireless Electrochemical Sensor Capsules for Real-Time Monitoring of Cell Secretomes and Culture Media in Tissue Growth Bioreactors.” Real-time bioprocess monitoring and control is needed for the scalable production and deployment of efficacious tissue engineered medical products (TEMPs) at reasonable cost.
Billyde Brown, the project's principal investigator, explained, “we are addressing this challenge by working with BioFabUSA, our partners at the Georgia Tech School of Materials Science and Engineering, the Marcus Center for Therapeutic Cell Characterization and Manufacturing, as well as Rockwell Automation, to develop a fully integrated, wireless, 3D-printed sensor ‘capsule’ to be used for in-situ multiplexed monitoring of critical quality attributes (CQAs). The targeted CQAs include pH, glucose, lactate, and select secreted biomarker concentrations from human mesenchymal stem cells – one of the most common cell types used in tissue engineering.”
In both biopharmaceutical and regenerative medicine industries, an urgent need remains for in-line sensor technology for quantitative real-time bioprocess monitoring and control. Unfortunately, many key CQAs are still monitored off-line or at-line using destructive testing or technologies of significant complexity and cost. In at-line measurement, the sample is typically withdrawn from a single location in the bioreactor and analyzed in close proximity to the process stream, whereas in off-line measurements, the sample is taken to a laboratory and the results are usually not returned in a timely manner for process control.
The Georgia Tech team has previously developed potentiometric sensors based on an extended gate field-effect-transistor (FET) topology whereby a separate gold electrode surface is functionalized with an analyte-specific layer that selectively reacts or binds with the chemical or biomolecule of interest. The charge associated with the attached analyte results in a potential change of the gold electrode. These sensors have previously been used to detect chemicals such as pH and lactate, as well as specific proteins/antibodies in a laboratory environment with accuracy and dynamic range equivalent to Surface Plasmon Resonance (SPR) and Enzyme-Linked Immunosorbent Assay (ELISA). One of the unique aspects of this system is that each sensor surface can be individually functionalized permitting multiplexed (simultaneous) detection of almost any number of different chemicals/biomolecules of interest.
In this project, the Georgia Tech team will integrate these sensors into a “capsule” device smaller than the size of a golf-ball and packaged in a 3D-printed waterproof and biocompatible polymer. The capsule will contain a multiplexed sensor chip, with sealed opening to facilitate interaction between the sensor chip and tissue culture environment, Li-polymer battery, and electronics for micro-control, data acquisition and wireless transmission of sensor data to the smartphone of a technician in charge of monitoring the bioreactor process. In addition, Georgia Tech will work with Rockwell to develop an IoT platform such that other permitted internet-connected devices can securely access the data via a cloud server. Another unique aspect of this technology is that multiple “capsules” could be deployed within a stirred tank bioreactor during high volume production of medical products with the ability to move efficiently throughout the bioreactor due to the mechanical forces of the impellors. This would allow for unprecedented simultaneous measurements at various points within the bioreactor, giving accurate representations of the homogeneity of key parameters over time thus achieving in-situ monitoring of CQAs with high spatial and temporal resolution.
Georgia Tech project leads include Billyde Brown, Ph.D., Kan Wang, Ph.D., and Eric Vogel, Ph.D. Brown is research faculty and director of manufacturing education programs at the Georgia Tech Manufacturing Institute (GTMI). Wang is lead researcher of additive manufacturing in the Bio-Engineering Research Laboratory at GTMI. Vogel is a professor at the School of Materials Science and Engineering and deputy director for the Institute of Electronics and Nanotechnology at Georgia Tech. The Georgia Tech project leads will also receive support and assistance from Carolyn Yeago, Ph.D., and Krishnendu Roy, Ph.D. whom are directors of the Marcus Center for Therapeutic Cell Characterization and Manufacturing (MC3M). Leading the project for Rockwell Automation is Wayne Charest, who also serves as a liaison between Rockwell and BioFabUSA.
“Being able to obtain real-time data on relevant biomarkers will be critical in advancing the field of tissue engineering,” said Stephanie Robichaud, technical project manager with the Advanced Regenerative Manufacturing Institute. “Getting this important information and being able to react to it quickly will result in more consistent manufacturing of a final product that meets its critical quality attributes.”
About the Georgia Institute of Technology
The Georgia Institute of Technology, also known as Georgia Tech, is one of the nation’s leading research universities — a university that embraces change while continually Creating the Next. The next generation of leaders. The next breakthrough startup company. The next lifesaving medical treatment.
Georgia Tech provides a focused, technologically based education to more than 36,000 undergraduate and graduate students. The Institute has many nationally recognized programs, all top-ranked by peers and publications alike, and is ranked among the nation’s top five public universities by U.S. News & World Report. It offers degrees through the Colleges of Computing, Design, Engineering, Sciences, the Scheller College of Business, and the Ivan Allen College of Liberal Arts. As a leading technological university, Georgia Tech has more than 100 centers focused on interdisciplinary research that consistently contribute vital research and innovation to American government, industry, and business. https://www.gatech.edu/
About Rockwell Automation
Rockwell Automation is the largest company in the world that is dedicated to industrial automation and information and is committed to enabling the next generation of smart manufacturing. Rockwell’s mission is to improve the quality of life by making the world more productive and sustainable.
https://www.rockwellautomation.com
About BioFabUSA
BioFabUSA is a DOD-funded Manufacturing USA Innovation Institute (MII) sustained by the Advanced Regenerative Manufacturing Institute (ARMI), a non-profit organization located in Manchester, New Hampshire. ARMI's mission is make practical the scalable, consistent, cost-effective manufacturing of tissue engineered medical products and tissue-related technologies, to benefit existing industries and grow new ones. https://www.armiusa.org/
Georgia Tech Manufacturing Institute
813 Ferst Drive, NW
Atlanta, GA 30332 USA
Media Relations Contact: Walter Rich (walter.rich@research.gatech.edu)
News Contact
Aug. 06, 2020
BioFabUSA, a Department of Defense-funded Manufacturing Innovation Institute within the Manufacturing USA network, has awarded the Georgia Institute of Technology and industry partner, Akron Biotech, a project titled, “Supply Chain and Process Modeling Algorithms, Methods, and Tools for Tissue Manufacturing and Distribution”. This project will address significant national supply chain issues related to distributing tissue engineered medical products (TEMPs) to U.S. patients in need.
The project aims to create the first simulation-based supply chain model for the rapidly evolving and future facing TEMPs industry, to minimize manufacturing and logistics costs and risks, incorporate Department of Defense (DOD) and other stakeholders’ perspectives into supply chain modeling, inform standards development, and support workforce development.
“Having a supply chain model will be instrumental in helping new and existing companies plan for the most efficient process flows, resource usage, and cost savings,” said Stephanie Robichaud, technical project manager with the Advanced Regenerative Manufacturing Institute. “Many startup companies do not realize some of the intricacies in managing their supply chain and many established companies realize the importance of it after experiencing inefficiencies. Having a model that these companies can use will help advance the field of tissue engineering as they plan for scale-up.”
According to Ben Wang, executive director of the Georgia Tech Manufacturing Institute (GTMI) and professor in the Stewart School of Industrial and Systems Engineering, “hundreds if not thousands of patients are waiting for tissues and organs in order to have a normal healthy life. Our project is a bold initiative to democratize distribution of replacement tissues and organs by streamlining national supply chains. This project will develop simulation-based tools to enhance the efficiency and resilience of the TEMPs supply chain, making these personalized medicines more affordable and more accessible.”
The growth of the TEMP industry is going to change the supply chain of medical tissues disruptively. To embrace this change, a system-level decision support tool is essential for adopting more cost-effective manufacturing processes and making better investment decisions. To ensure successful commercialization and adoption of this new supply chain decision support tool, the project team will engage multiple stakeholders including DOD, government, regulatory bodies, standards setting organizations, patients, industry, academia, policy experts, education and workforce development experts.
Georgia Tech project leads include Ben Wang, Ph.D., Chelsea C. White III, Ph.D, and Kan Wang, Ph.D. Ben Wang is Gwaltney Chair in Manufacturing Systems, professor in the Stewart School of Industrial & Systems Engineering and School of Materials Science and Engineering at Georgia Tech. In addition, he serves as executive director of the Georgia Tech Manufacturing Institute (GTMI). Chelsea C. White III is the Schneider National Chair in Transportation and Logistics and professor in the H. Milton Stewart School of Industrial and Systems Engineering at Georgia Tech. Kan Wang is lead researcher of additive manufacturing in the Bio-Engineering Research Laboratory at GTMI.
Leading the project for Akron Biotech is Ezequiel Zylberberg, Ph.D, who is vice president of product development and planning. According to Ezequiel, “the future of regenerative medicine depends on more than our ability to address the scientific challenges of generating the next generation of advanced therapies. Advancing these novel treatments in a way that is scalable will require significant advances in manufacturing innovation. We are eager to collaborate with our colleagues at Georgia Tech, at BioFab USA, and throughout the regenerative medicine industry to confront the challenge of scalability and supply chain resilience through this modelling effort.”
About the Georgia Institute of Technology
The Georgia Institute of Technology, also known as Georgia Tech, is one of the nation’s leading research universities — a university that embraces change while continually Creating the Next. The next generation of leaders. The next breakthrough startup company. The next lifesaving medical treatment.
Georgia Tech provides a focused, technologically based education to more than 36,000 undergraduate and graduate students. The Institute has many nationally recognized programs, all top-ranked by peers and publications alike, and is ranked among the nation’s top five public universities by U.S. News & World Report. It offers degrees through the Colleges of Computing, Design, Engineering, Sciences, the Scheller College of Business, and the Ivan Allen College of Liberal Arts. As a leading technological university, Georgia Tech has more than 100 centers focused on interdisciplinary research that consistently contribute vital research and innovation to American government, industry, and business. https://www.gatech.edu/
About Akron Biotech
Akron is a leading materials manufacturer and services provider to the regenerative medicine industry, accelerating the development and commercialization of advanced therapies. Founded in 2006, Akron is an ISO 13485-certified company that operates in line with cGMPs and international standards, enabling advanced therapy developers to de-risk their supply chains and facilitate regulatory approval. The company's unique business model emphasizes knowledge, flexibility and unparalleled service—from development through to commercialization. For more information, please visit www.akronbiotech.com.
About BioFabUSA
BioFabUSA, is a DOD-funded Manufacturing USA Innovation Institute (MII) sustained by the Advanced Regenerative Manufacturing Institute (ARMI) is a non-profit organization located in Manchester, New Hampshire. ARMI's mission is to make practical the scalable, consistent, cost-effective manufacturing of tissue engineered medical products and tissue-related technologies, to benefit existing industries and grow new ones. https://www.armiusa.org/
Georgia Tech Manufacturing Institute
813 Ferst Drive, NW
Atlanta, GA 30332 USA
Media Relations Contact: Walter Rich (walter.rich@research.gatech.edu)
News Contact
Jul. 28, 2020
Personal initiatives by a pediatrician and by researchers to make face shields for medical workers have transformed into an industry collaboration that by June had delivered 1.8 million shields to hospitals and other organizations around the country with plans to produce 2.5 million all total. A $2 million donation from Aflac Incorporated for personal protective equipment (PPE) financed the bulk of the shields.
To make it happen, a team of researchers and industry partners convened at the Global Center for Medical Innovation (GCMI), a Georgia Tech-affiliated nonprofit that guides new experimental medical solutions to market. The group combined the physician’s vision with the researchers’ original designs, adjusted them to pass FDA emergency guidelines, and then coordinated mass production and distribution.
A physician’s wisdom
The project grew wings in mid-March, after Dr. Joanna Newton became concerned that the nationwide shortage of PPE was leaving healthcare workers across the country vulnerable. Newton is a physician specializing in improving healthcare safety through technology at Children’s Healthcare of Atlanta, and she was already collaborating with Georgia Tech on other projects.
She grabbed the phone to leverage the connection.
“I called Sherry Farrugia to tell her about my idea to 3D-print PPE. We needed to quickly find a solution for the PPE shortage around the country, and I knew we had the right team here in Atlanta to help,” said Newton, a pediatric hematologist/oncologist at the Aflac Cancer and Blood Disorders Center of Children’s.
“The situation was urgent, and I knew who would have the right expertise to get this done,” said Farrugia, chief operating officer and strategy officer of Children’s Healthcare of Atlanta Pediatric Technology Center, which is part of Georgia Tech.
Farrugia had Newton present her idea at GCMI to researchers, advisors, and industry partners who immediately put together a team to address the need for face shields to protect healthcare workers from droplets containing the coronavirus. She also discussed the need with Devesh Ranjan, associate chair of the George W. Woodruff School of Mechanical Engineering, who suggested connecting the effort to a parallel initiative in that school.
Bringing in engineers
At the same time, along with Ranjan, Sam Graham, chair of the George W. Woodruff School of Mechanical Engineering, and Susan Margulies, chair of the Wallace H. Coulter Department of Biomedical Engineering, were coordinating efforts across campus to develop various medical devices in response to the pandemic. Graham, Margulies, and Ranjan quickly connected GCMI with Christopher Saldana and Saad Bhamla, faculty members in Georgia Tech’s College of Engineering, who were leading an simultaneous effort to address the face shield problem with their students using rapid fabrication techniques like 3-D printing, laser cutting, and waterjet cutting.
“The Georgia Tech mechanical engineering team used rapid fabrication equipment and quickly produced multiple face shield designs that could be manufactured in high volumes for the rapid response environment that Covid-19 required,” Saldana said.
Making a few thousand shields in a lab had likely already saved lives, but the Georgia Tech researchers and GCMI put their designs on the internet, where they have been downloaded thousands of times by organizations manufacturing them around the world. And the manufacturing partners they engaged have been turning out hundreds of thousands of shields to save many more lives.
“You may need 45 minutes for a headband with a 3D printer, but manufacturers turn out six of them every 19 seconds. Then making a million face shields becomes a real possibility,” said Mike Fisher, who leads product development at GCMI.
GCMI opened a GoFundMe page, which brought in $20,000, and then engaged their first manufacturing partner, Delta Air Lines.
A manufacturing explosion
“Delta converted one of their groups from manufacturing airplane interiors to doing the face shields. They started off by manufacturing 6,000 shields, and that got the momentum going,” Leiter said. “Two thousand shields went to Mount Sinai Hospital in New York; 2,000 went to Piedmont Healthcare in Atlanta; and 2,000 went to Children’s Healthcare of Atlanta.”
Things began to snowball.
Graham engaged Siemens Industries to fulfill a face shield order from the Georgia Emergency Management Agency (GEMA) for distribution in Georgia. Partners from ExxonMobil began looking for more potential manufacturers. And Aflac contacted Children’s looking for worthy Covid-19 related efforts to support.
“We asked for a donation of $500,000 for manufacturers to retool their operations. Aflac made a gift of $2 million to GCMI to promote the production of PPE,” Farrugia said. “We were able to buy tooling for an automotive plastics manufacturer called Quality Model in South Carolina, and they have made over 750,000 face shields so far.”
GCMI won a bid from the Federal Emergency Management Agency (FEMA) for 1,141,600 face shields, which are being made by Quality Model, where ExxonMobil helped rearrange production lines for shields.
Siemens made an additional 100,000 shields from Aflac’s gift, which is also being used to purchase existing PPE to donate to healthcare workers. Kia Motors quickly produced an initial 15,000 shields, which the company financed itself.
“Kia got the open source design from the Georgia Tech website and ran with it on their own,” Saldana said.
These partners are delivering the following number of shields: Quality Model, 1,251,600; Kia Motors, 300,000; Siemens Industries, 205,000; Delta Air Lines, 106,100; Georgia Tech, 20,000; and EIS, 15,000. And more are still to come.
The shields went across the country, from hospitals in New York City to Prisma Health in South Carolina, to nursing homes in the Pensacola area, and to rural Louisiana and Mississippi, Leiter said.
Thanks in large part to Aflac’s gift, GCMI and Farrugia are coordinating with partners, including Georgia Tech engineers, to produce N95 masks, hospital gowns, and hand sanitizer, all redesigned for the Covid-19 age.
Research News
Georgia Institute of Technology
177 North Avenue
Atlanta, Georgia 30332-0181 USA
Media Relations Assistance: John Toon (404-894-6986) (jtoon@gatech.edu).
Writer: Ben Brumfield
News Contact
John Toon
Research News
(404) 894-6986
Jul. 01, 2020
Pagination
- Previous page
- 4 Page 4
- Next page