Apr. 11, 2024
The Center for Sustainable Communities Research and Education (SCoRE — formerly SLS), in collaboration with the Strategic Energy Institute (SEI), the Brook Byers Institute for Sustainable Systems (BBISS), the Renewable Bioproducts Institute (RBI), and the Social Equity and Environmental Engineering Lab (SEEEL), launched the Energy Equity, Environmental Justice, and Community Engagement Faculty Fellows Program in November 2023. In this program, Georgia Tech faculty learn how to work with communities, bringing together their academic knowledge and the local expertise of communities that has been developed through lived experience and long-standing social action.
The inaugural fellows include 24 Georgia Tech faculty from five Colleges, as well as a faculty colleague from Georgia Gwinnett College and a partner from the Southeast Energy Efficiency Alliance, who are building relationships with each other and with community partners in the areas of energy equity and environmental justice. Since the launch, they have engaged in a wide array of events, including community benefit and development workshops, site visits to community-based organizations across the Atlanta region, and university-community gatherings and symposia.
The program is expected to result in both collective and individual deliverables. Collective deliverables include the development of network mapping tools to facilitate collaborations inside and outside Georgia Tech, a set of principles for conducting community-engaged research, a reflective essay on faculty training for community-engaged research, and ideas for future activities to facilitate university-community and interdisciplinary team formation. Fellows individually determine their deliverables, which run the gamut from exploring partnerships for a specific research project to writing a societal impact statement for a tenure package.
More broadly, the program aims to grow Georgia Tech’s collaborative expertise in community-engaged research by forming a supportive network of faculty interested in community-engaged sustainability research and education.
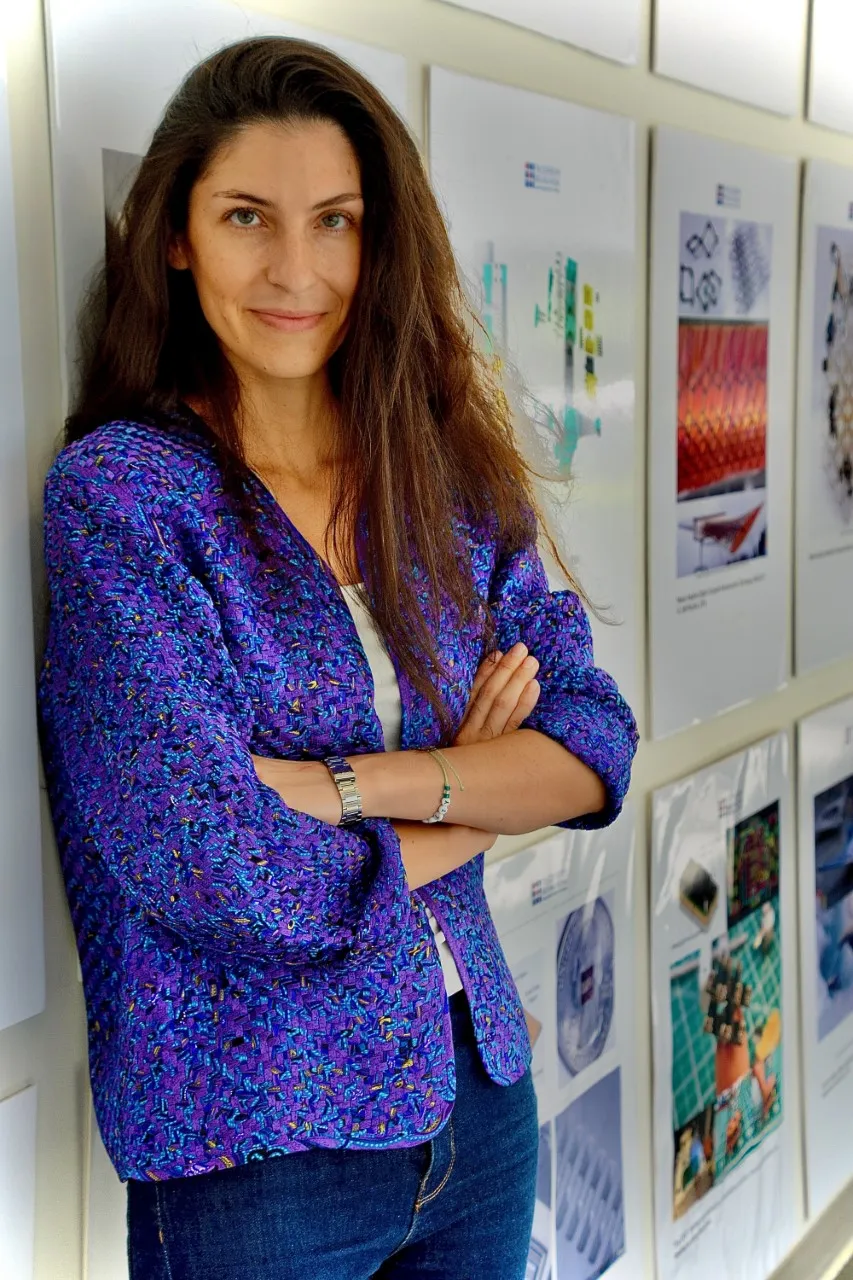
Faculty Affiliate: Patritsia Stathatou, Research Scientist, Renewable Bioproducts Institute, Georgia Tech
Sustainable energy sources and environmental justice go hand in hand. Although such technologies aim to minimize environmental impacts of modern societies, without considering issues of environmental justice and energy equity, these solutions can inadvertently perpetuate disparities by disproportionately benefiting certain communities while harming others. Bridging the gap between technological advancements and community benefits is paramount to creating an equitable energy future for all.
This program provides a unique opportunity to explore these interconnections, enhancing my knowledge in integrating community values and concerns into my research on alternative fuels and renewable energy sources. I am particularly excited about the hands-on approach of the program, which emphasizes listening sessions and workshops, allowing fellows to gain direct insights from various stakeholders. I hope that, through active participation in these sessions, I can further my understanding of the challenges faced by local communities and incorporate these insights into actionable solutions in my research.
In my project, I'm in a group crafting a reflective essay about our experiences with Community Engaged Research training. Our goal is to translate the insights gained from this pilot program into a publishable piece. Additionally, I'm acquiring valuable insights into the development of Broader Impact Statements and Community Benefits Plans, crucial parts of proposals for securing federal funding from NSF and DoE, respectively.
Faculty Affiliate: Sofia Perez-Guzman, Assistant Professor, School of Civil and Environmental Engineering, Georgia Tech
The fellowship program has been a fantastic experience. I never imagined how much I would learn from this program about properly engaging with communities. As researchers, we might think we want to hear the needs that communities face to provide them with solutions. That is different than the way community-driven research should work. I’ve learned that researchers need to gain the communities’ trust, be present and participate in their events, and, more importantly, work at their pace and for their interests rather than push our research agendas for our professional benefit. I know there is still a lot more I must continue learning, but what I’ve learned so far has been an eye-opener that is making me rethink how to approach my research and its social aspect.
My project focuses on the social performance of supply chains, and I am seeking to put more emphasis on the “social” part of my research by making it more community-driven. That is why I applied for the fellowship. I am advancing two current projects as part of the fellowship. One relates to increasing food accessibility to vulnerable populations via community-driven freight transportation solutions. I want to bring food closer to people and do it by co-designing solutions with the communities. The second project relates to forming a team to pursue research on enhancing community resilience to extreme weather events for the mobility of people and goods. The fellowship and a Sustainability Next seed grant from BBISS are helping me move forward with this project.
News Contact
Priya Devarajan
Research Communications Program Manager || SEI | RBI
Mar. 18, 2024
A new study by Associate Professor Omar Isaac Asensio and a team of students in Georgia Tech’s School of Public Policy finds that federal housing policies accelerate energy efficiency participation among low- and moderate-income households — even when those policies don’t directly address energy efficiency.
The research, published in Nature Sustainability, shows how community development block grants from the U.S. Department of Housing and Urban Development (HUD) generated an average of 5% to 11% energy savings in economically burdened households in Albany. The savings equate to the cost of roughly two months of groceries per household per year.
"These housing participants who didn't come in thinking about energy efficiency saved anywhere from $75 to $482 per year in energy bills," Asensio said. "Those are meaningful savings that really impact people. So, we ended up finding very significant hidden social benefits from these policies that were previously unknown."
https://youtu.be/eWqOFj9qRxw
The findings are surprising because HUD grants do not specifically target energy efficiency or sustainability measures in exchange for governmental assistance. Instead, they are given at the discretion of the local government to residents facing housing emergencies such as deteriorating roofs or broken HVAC systems in the hot summer. Because of the high amount of deferred maintenance in these homes, the fixes have a spillover effect of significantly reducing energy use — for example, by adopting more efficient technologies and bringing structures up to building codes — and saving money for people who receive them.
The multidisciplinary research team in Asensio’s Data Science & Policy Lab, including current and former Public Policy students Olga Churkina and Becky D. Rafter and industrial engineering alumna Kira E. O'Hare, also found that the cost-effectiveness of housing-based interventions rivals standalone energy efficiency policies, offering a promising alternative for reaching marginalized communities.
"For decades, we’ve struggled to get meaningful participation with conventional policies in these lower and moderate-income communities, including among renters and people in multi-family homes,” Asensio said. "Using housing block grants as an entry strategy to drive efficiency is an important policy innovation.”
With support from the National Science Foundation, ESRI, Inc., and the Georgia Smart Communities Challenge, Asensio and his co-authors spent nearly four years collecting, cleaning, and combining Albany's previously siloed city data into one community analytics repository. They linked records for 5.9 million utility bills per month from 2004 to 2019, allowing them to see long-run impacts of policy intervention, energy consumption, and payments by household — an uncommonly granular level of data.
"Overall, HUD-funded block grants in Albany reduced electricity use by 4.72 million kilowatt hours over the study period versus the control group," the researchers wrote. "The reduction in non-baseload emissions is equivalent to 3.70 million pounds of coal not being burned or the carbon sequestered by 3,695 acres of forest."
Asensio's research is timely because the Southeast has some of the country's highest energy-burdened households. In the U.S., spending over 6% of net income on energy is considered a burden. In Albany, renters' and homeowners' energy costs can surpass ten or even 20% of household budgets, Asensio said, and many housing applicants are elderly and on fixed incomes.
Unlike conventional energy initiatives that are reliant on self-selection, housing programs can provide a more equitable and localized strategy. That's because "most of the standalone policies for energy efficiency have two main outcomes," Asensio said. "First, the programs generally attract more affluent and informed homeowners, in which case, questions arise as to whether this might be a good use of public funds. Second, when these policies are restricted to certain income eligibility limits, we don't get enough participation from lower-income residents for a long list of reasons. So, reaching low- and moderate-income households has become a fundamental challenge."
In contrast, housing block grants naturally target a broader range of residents with high energy burdens and help circumvent the problem of low participation. Rather than trying to market an energy-saving offer to people who aren't interested or are distrustful of the government, HUD grants have long waiting lists.
"There are thousands and thousands of communities that look very much like Albany within and outside of major metro areas,” Asensio said. "This is a relatively untapped opportunity for driving energy efficiency within households who may not necessarily have an awareness of or interest in energy efficiency measures.”
The paper, “Housing Policies and Energy Efficiency Spillovers in Low and Moderate Income Communities,” was published online in Nature Sustainability on March 18. It is available at https://doi.org/10.1038/s41893-024-01314-w. This work was partially supported by awards from the National Science Foundation (Award No. 1945332), ESRI, Inc., the Georgia Smart Communities Challenge, and the Institute for the Study of Business in Global Society at Harvard Business School.
News Contact
Di Minardi
Ivan Allen College of Liberal Arts
Mar. 14, 2024
In January, Georgia Tech researchers were awarded three grants as a part of the Department of Energy’s Industrial Efficiency and Decarbonization multi-topic funding. The awards include 49 high-impact, applied research, development, and pilot-scale technology validation and demonstration projects that will reduce energy usage and greenhouse gas emissions in conjunction with cross-sector industrial decarbonization approaches.
The Georgia Tech funding includes a project, in the topic area of Decarbonizing Forest Products, on innovative refining, paper forming, and drying to eliminate CO2 emissions from paper machines. Funded at $3.1 million, the project is led by Carson Meredith, professor and James Harris Faculty Fellow in the School of Chemical and Biomolecular Engineering and executive director of the Renewable Bioproducts Institute (RBI). Collaborators include co-PI Cyrus Aidun, professor of mechanical engineering; Patritsia Stathatou, research scientist at RBI; and Aruna Weerasakura, senior research engineer. External collaborators include Fort Valley State University, the National Renewable Energy Laboratory, and several RBI member companies.
Meredith’s project focuses on decarbonization in energy-intensive drying, paper forming, and pulping processes and will combine recent deflocculation breakthroughs in fiber refining with low-water, multiphase paper forming. The innovations will facilitate the cost-effective implementation of advanced electrical drying technologies in the paper industry. By taking advantage of the increasing fraction of non-fossil electricity in the U.S., electrified drying, if implemented partially (50%), has the potential to reduce the generation of non-biogenic emissions by over 10 million metric tons of CO2e annually.
"I am excited because the new project will utilize the multiphase forming laboratory that is under construction in the Paper Tricentennial Building, representing the first major expansion in lab space there since the 1990s,” said Meredith.
Valerie Thomas, the Anderson-Interface Chair of Natural Systems and professor of industrial and systems engineering and public policy, is a co-PI in a $1.45 million project titled “Mild Co-Solvent Pulping to Decarbonize the Paper and Forest Products Sector,“ led by the University of California, Riverside.
Thomas’ project, also under the topic area of Decarbonizing Forest Products, aims to enhance Co-solvent Enhanced Lignocellulosic Fractionation (CELF) technology into a more environmentally sustainable alternative to traditional kraft pulping. CELF technology will be applied to optimize the production of dissolving pulp used in the manufacturing of extruded textile fibers and will also produce dissolving lignin as a by-product that can serve as a natural resin binder or a renewable ingredient for producing industrial adhesives and binders. This technology has the potential to reduce carbon intensity by 50 – 75% and operating costs by 10 – 20%.
Tim Lieuwen, David S. Lewis Jr. Chair and professor in aerospace engineering and executive director of the Strategic Energy Institute, is co-PI along with Vishal Acharya, principal research engineer and Benjamin Emerson, principal research engineer at Georgia Tech in a $3.25 million project titled “Omnivore Combustion System,” led by GTI Energy, an Illinois-based technology company.
Lieuwen’s project, under the topic area of Low-Carbon Fuels Utilization R&D, will design and demonstrate a scaled, adaptable omnivore combustion system (OCS) that can accommodate a continuously varying blend of low-carbon fuels with ultra-low nitrous oxide emissions, including natural gas-hydrogen blends, syngas, and biogas. The project will demonstrate a full-scale OCS for at least 100 hours and will focus on three aspects — improving performance, operation stability and safety, and fuel flexibility — and can potentially be used for industrial furnace applications in high carbon-emitting industries.
“The industrial sector is large in both its significance for our economy and its negative climate impacts, and each of these projects addresses significant challenges for the decarbonization of this critical sector,” Lieuwen said.
The projects are part of DOE’s Technologies for Industrial Emissions Reduction Development (TIEReD) Program, which invests in fundamental science, research, development, and initial pilot-scale demonstrations projects to decarbonize the industrial sector — currently responsible for a third of the nation’s greenhouse gas emissions.
News Contact
Priya Devarajan || Research Programs Communications Manager || RBI || SEI
Mar. 12, 2024
Cicadas are the soundtrack of summer, but their pee is more special than their music. Rather than sprinkling droplets, they emit jets of urine from their small frames. For years, Georgia Tech researchers have wanted to understand the cicada’s unique urination.
Cicadas are the soundtrack of summer, but their pee is more special than their music. Rather than sprinkling droplets, they emit jets of urine from their small frames. For years, Georgia Tech researchers have wanted to understand the cicada’s unique urination.
Saad Bhamla, an assistant professor in the School of Chemical and Biochemical Engineering, and his research group hoped for an opportunity to study a cicada’s fluid excretion. However, while cicadas are easily heard, they hide in trees, making them hard to observe. As such, seeing a cicada pee is an event. Bhamla’s team had only watched the process on YouTube.
Then, while doing fieldwork in Peru, the team got lucky: They saw numerous cicadas in a tree, peeing.
Read more about what they discovered at Georgia Tech Research News.
News Contact
Tess Malone, Senior Research Writer/Editor
tess.malone@gatech.edu
Mar. 07, 2024
Matthew McDowell, Woodruff Faculty Fellow and associate professor in the George W. Woodruff School of Mechanical Engineering and the School of Materials Science and Engineering and initiative lead for energy storage at the Strategic Energy Institute, has received $1.3 million in funding through the Pioneering Railroad, Oceanic, and Plane Electrification with 1K energy storage systems (PROPEL-1K) program. Aimed at accelerating the electrification of the aviation, railroad, and maritime transportation sectors, PROPEL-1K is one of the latest ARPA-E grants with projects to develop energy storage systems that can achieve over 1,000 watt-hour per kilogram and 1,000 watt-hour per liter. These technologies will improve energy density fourfold over current technologies.
Inspired by fuel injectors in internal combustion engines and conventional flow batteries, McDowell’s project will advance an alkali hydroxide triple phase flow battery to enable reversible operation of ultrahigh-energy density battery chemistries. The project’s proposed design will increase energy density by leveraging innovative pumping and handling of molten alkali metal and hydroxide species to maximize the volume of reactants over inactive components.
McDowell will work with Asegun Henry, associate professor in the Department of Mechanical Engineering at the Massachusetts Institute of Technology (MIT). Prior to MIT, Henry was an assistant professor in the George W. Woodruff School of Mechanical Engineering at Georgia Tech.
Created in 2007, the Advanced Research Projects Agency-Energy (ARPA-E) in the Department of Energy advances high-potential, high-impact energy technologies. The agency focuses on transformational energy projects that can be meaningfully advanced with a small amount of funding over a defined period through a streamlined awards process that enables quick action and catalyzes cutting-edge areas of energy research.
News Contact
Priya Devarajan | SEI Communications Program Manager
Feb. 21, 2024
Energy is everywhere, affecting everything, all the time. And it can be manipulated and converted into the kind of energy that we depend on as a civilization. But transforming this ambient energy (the result of gyrating atoms and molecules) into something we can plug into and use when we need it requires specific materials.
These energy materials — some natural, some manufactured, some a combination — facilitate the conversion or transmission of energy. They also play an essential role in how we store energy, how we reduce power consumption, and how we develop cleaner, efficient energy solutions.
“Advanced materials and clean energy technologies are tightly connected, and at Georgia Tech we’ve been making major investments in people and facilities in batteries, solar energy, and hydrogen, for several decades,” said Tim Lieuwen, the David S. Lewis Jr. Chair and professor of aerospace engineering, and executive director of Georgia Tech’s Strategic Energy Institute (SEI).
That research synergy is the underpinning of Georgia Tech Energy Materials Day (March 27), a gathering of people from academia, government, and industry, co-hosted by SEI, the Institute for Materials (IMat), and the Georgia Tech Advanced Battery Center. This event aims to build on the momentum created by Georgia Tech Battery Day, held in March 2023, which drew more than 230 energy researchers and industry representatives.
“We thought it would be a good idea to expand on the Battery Day idea and showcase a wide range of research and expertise in other areas, such as solar energy and clean fuels, in addition to what we’re doing in batteries and energy storage,” said Matt McDowell, associate professor in the George W. Woodruff School of Mechanical Engineering and the School of Materials Science and Engineering (MSE), and co-director, with Gleb Yushin, of the Advanced Battery Center.
Energy Materials Day will bring together experts from academia, government, and industry to discuss and accelerate research in three key areas: battery materials and technologies, photovoltaics and the grid, and materials for carbon-neutral fuel production, “all of which are crucial for driving the clean energy transition,” noted Eric Vogel, executive director of IMat and the Hightower Professor of Materials Science and Engineering.
“Georgia Tech is leading the charge in research in these three areas,” he said. “And we’re excited to unite so many experts to spark the important discussions that will help us advance our nation’s path to net-zero emissions.”
Building an Energy Hub
Energy Materials Day is part of an ongoing, long-range effort to position Georgia Tech, and Georgia, as a go-to location for modern energy companies. So far, the message seems to be landing. Georgia has had more than $28 billion invested or announced in electric vehicle-related projects since 2020. And Georgia Tech was recently ranked by U.S. News & World Report as the top public university for energy research.
Georgia has become a major player in solar energy, also, with the announcement last year of a $2.5 billion plant being developed by Korean solar company Hanwha Qcells, taking advantage of President Biden’s climate policies. Qcells’ global chief technology officer, Danielle Merfeld, a member of SEI’s External Advisory Board, will be the keynote speaker for Energy Materials Day.
“Growing these industry relationships, building trust through collaborations with industry — these have been strong motivations in our efforts to create a hub here in Atlanta,” said Yushin, professor in MSE and co-founder of Sila Nanotechnologies, a battery materials startup valued at more than $3 billion.
McDowell and Yushin are leading the battery initiative for Energy Materials Day and they’ll be among 12 experts making presentations on battery materials and technologies, including six from Georgia Tech and four from industry. In addition to the formal sessions and presentations, there will also be an opportunity for networking.
“I think Georgia Tech has a responsibility to help grow a manufacturing ecosystem,” McDowell said. “We have the research and educational experience and expertise that companies need, and we’re working to coordinate our efforts with industry.”
Marta Hatzell, associate professor of mechanical engineering and chemical and biomolecular engineering, is leading the carbon-neutral fuel production portion of the event, while Juan-Pablo Correa-Baena, assistant professor in MSE, is leading the photovoltaics initiative.
They’ll be joined by a host of experts from Georgia Tech and institutes across the country, “some of the top thought leaders in their fields,” said Correa-Baena, whose lab has spent years optimizing a semiconductor material for solar energy conversion.
“Over the past decade, we have been working to achieve high efficiencies in solar panels based on a new, low-cost material called halide perovskites,” he said. His lab recently discovered how to prevent the chemical interactions that can degrade it. “It’s kind of a miracle material, and we want to increase its lifespan, make it more robust and commercially relevant.”
While Correa-Baena is working to revolutionize solar energy, Hatzell’s lab is designing materials to clean up the manufacturing of clean fuels.
“We’re interested in decarbonizing the industrial sector, through the production of carbon-neutral fuels,” said Hatzell, whose lab is designing new materials to make clean ammonia and hydrogen, both of which have the potential to play a major role in a carbon-free fuel system, without using fossil fuels as the feedstock. “We’re also working on a collaborative project focusing on assessing the economics of clean ammonia on a larger, global scale.”
The hope for Energy Materials Day is that other collaborations will be fostered as industry’s needs and the research enterprise collide in one place — Georgia Tech’s Exhibition Hall — over one day. The event is part of what Yushin called “the snowball effect.”
“You attract a new company to the region, and then another,” he said. “If we want to boost domestic production and supply chains, we must roll like a snowball gathering momentum. Education is a significant part of that effect. To build this new technology and new facilities for a new industry, you need trained, talented engineers. And we’ve got plenty of those. Georgia Tech can become the single point of contact, helping companies solve the technical challenges in a new age of clean energy.”
News Contact
Feb. 15, 2024
Demand for critical minerals and rare earth elements is rapidly increasing as the world accelerates toward clean energy transitions. Concerns about price volatility, supply security, and geopolitics arise as reducing emissions and ensuring resilient and secure energy systems become increasingly crucial.
To address this important area, 45 participants from academia, government, industry, and national labs gathered at the University of Georgia for the inaugural Georgia partnerships for Essential Minerals (GEMs) Workshop. The workshop was the first in a series of critical mineral conversations planned by the collaborators of the workshop. The first GEMs Workshop focused on the critical mineral potential in Georgia’s kaolin mining industry.
Key workshop conveners included W. Crawford Elliott, associate professor of chemistry and geosciences at Georgia State University; Lee R. Lemke, secretary and executive vice president of the Georgia Mining Association; Paul A. Schroeder, professor in clay minerology at the University of Georgia; and Yuanzhi Tang, associate professor in the School of Earth and Atmospheric Sciences at Georgia Tech.
Representatives from more than 20 companies, the Environmental Protection Agency, U.S. Geological Survey, Georgia Environmental Protection Division, and Savannah River National Laboratory, as well as faculty members and students from Georgia’s three R1 universities participated in the day-long workshop. Speaker sessions and panel discussions addressed:
- Developing a state and regional ecosystem demonstrating a critical mineral supply chain from resources to solutions to end users.
- A strong emphasis on workforce training for this emerging industry.
- Establishing a regional critical mineral consortium to facilitate resource exploration, characterization, processing, and utilization.
- Creating official industry-university collaborations that included internships, field trips, curricular training, R&D collaboration, and stakeholder liaisons.
Workshop organizers plan to reconvene in six months to continue conversations and build momentum on critical minerals research, from supplies to workforce training and beyond.
News Contact
Priya Devarajan, Georgia Institute of Technology
Alan Flurry, University of Georgia
Anna Varela, Georgia State University
Feb. 15, 2024
Demand for critical minerals and rare earth elements is rapidly increasing as the world accelerates toward clean energy transitions. Concerns about price volatility, supply security, and geopolitics arise as reducing emissions and ensuring resilient and secure energy systems become increasingly crucial.
To address this important area, 45 participants from academia, government, industry, and national labs gathered at the University of Georgia for the inaugural Georgia partnerships for Essential Minerals (GEMs) Workshop. The workshop was the first in a series of critical mineral conversations planned by the collaborators of the workshop. The first GEMs Workshop focused on the critical mineral potential in Georgia’s kaolin mining industry.
Key workshop conveners included W. Crawford Elliott, associate professor of chemistry and geosciences at Georgia State University; Lee R. Lemke, secretary and executive vice president of the Georgia Mining Association; Paul A. Schroeder, professor in clay minerology at the University of Georgia; and Yuanzhi Tang, associate professor in the School of Earth and Atmospheric Sciences at Georgia Tech.
Representatives from more than 20 companies, the Environmental Protection Agency, U.S. Geological Survey, Georgia Environmental Protection Division, and Savannah River National Laboratory, as well as faculty members and students from Georgia’s three R1 universities participated in the day-long workshop. Speaker sessions and panel discussions addressed:
- Developing a state and regional ecosystem demonstrating a critical mineral supply chain from resources to solutions to end users.
- A strong emphasis on workforce training for this emerging industry.
- Establishing a regional critical mineral consortium to facilitate resource exploration, characterization, processing, and utilization.
- Creating official industry-university collaborations that included internships, field trips, curricular training, R&D collaboration, and stakeholder liaisons.
Workshop organizers plan to reconvene in six months to continue conversations and build momentum on critical minerals research, from supplies to workforce training and beyond.
News Contact
Priya Devarajan, Georgia Institute of Technology
Alan Flurry, University of Georgia
Anna Varela, Georgia State University
Feb. 13, 2024
Mechanical engineering, in the broadest sense of the discipline, touches a vast array of processes and systems, encompassing familiar industries and niche startups. Rapid technology advances mean engineering skills and methods change frequently to adapt to newer materials, tools, or customer needs. At its core, however, the intersection of design and innovation drives engineering, shaping the future of products and manufacturing processes. At the forefront of this intersection is the George W. Woodruff School of Mechanical Engineering at Georgia Tech, well known for its commitment to design education and unique approach to understanding the crucial role design plays in educating future engineers.
News Contact
Ian Sargent
Feb. 12, 2024
The University of Waterloo and the Board of Regents of the University System of Georgia, representing Georgia Institute of Technology (Georgia Tech), have officially entered a Memorandum of Understanding (MOU) to strengthen academic and research ties between the two institutions. The MOU signifies a commitment to fostering collaborative initiatives in research, education, and other areas of mutual interest. Both universities, recognized for their global impact and innovation, are eager to embark on this journey of cooperation.
Charmaine Dean, Vice-President of Research & International, shared, “The University of Waterloo is pleased to embark on a new collaboration with Georgia Tech, featuring faculty and student exchanges, joint research projects, dual degrees, and conferences. Strengthening ties between our institutions through this collaboration creates a dynamic environment for our faculty and students to foster innovation in many areas of mutual excellence.”
“Georgia Tech is excited to see its NSF AI Institute for Advances in Optimization (AI4OPT), under the leadership of Prof. Pascal Van Hentenryck, partner with experts from the Waterloo Artificial Intelligence Institute of the University of Waterloo. I am really looking forward to the impact that this partnership will have in advancing the fundamental knowledge of AI, in further expanding its applications, and in enabling its wider adoption,” noted Prof. Bernard Kippelen, Vice Provost for International Initiatives at Georgia Tech.
This collaboration is poised to elevate the academic and research landscape of both institutions, promoting global engagement and creating opportunities for students and faculty to thrive in an interconnected world.
News Contact
Breon Martin
Pagination
- Previous page
- 13 Page 13
- Next page