Jan. 18, 2012
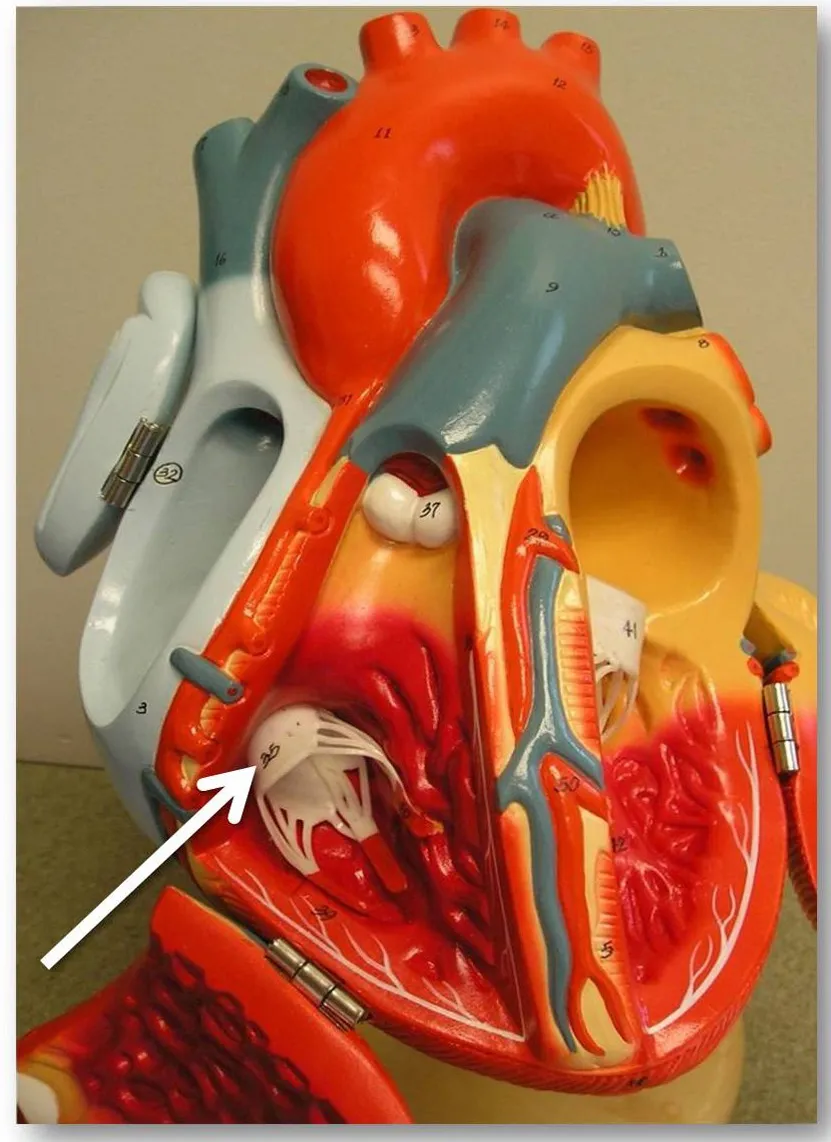
An estimated 1.6 million Americans suffer moderate to severeleakage through their tricuspid valves, which are complex structures that allowblood to flow from the heart’s upper right chamber to the ventricle. If leftuntreated, severe leakage can affect an individual’s quality of life and can evenlead to death.
A new study finds that the anatomy of the heart’s tricuspidvalve can be used to predict the severity of leakage in the valve, which is acondition called tricuspid regurgitation. The study, conducted by researchersfrom the Georgia Institute of Technology and Emory University, found that pulmonaryarterial pressure, the size of the valve opening and papillary muscle position measurementscould be used to predict the severity of an individual’s tricuspidregurgitation.
“By being able to identify and measure an individual’sparticular tricuspid valve anatomical features that we have shown arecorrelated with increased leakage, clinicians should be able to better target their repair efforts and create moredurable repairs,” said Ajit Yoganathan, Regents’ professor in theWallace H. Coulter Department of Biomedical Engineering at Georgia Tech andEmory University.
The study was published in the January issue of the journal Circulation: Cardiovascular Imaging. Funding for this work wasprovided by the American Heart Association and a donation from Tom and ShirleyGurley.
Yoganathan and recent Coulter Department doctoral graduate ErinSpinner teamed with Stamatios Lerakis, a professor of medicine (cardiology), radiologyand imaging sciences at Emory University, to non-invasively collect 3-Dechocardiograms from 64 individuals who exhibited assorted grades of tricuspid leakage.Subjects included 20 individuals with “trace,” 13 with “mild,” 17 with “moderate”and 14 with “severe” tricuspid regurgitation. The subjects with “mild” to“severe” leakage exhibited a mix of isolated right, isolated left, and bothright and left ventricle dilation.
From the 3-D echocardiography images of the heart theycollected, the researchers measured (1) the area of the annulus, which is thefibrous ring that surrounds the tricuspid valve opening; (2) the distancebetween the annulus and the three right ventricle papillary muscles, which keepthe valve shut when the ventricle contracts; and (3) the position of the papillarymuscles with respect to the center of the annulus. The clinicians also measuredpulmonary arterial pressure using standard clinical methods and assessed thegrade of tricuspid regurgitation from “trace” to “severe” with color Dopplerimaging.
In collaboration with Emir Veledar, an assistant professorand statistician in the Rollins School of Public Health at Emory University, theresearchers found statistical differences between individuals with ventricular dilationand the control subjects in the parameters of pulmonary arterial pressure,annulus area and papillary muscle displacement. They also found that all three factors were correlated with the gradeof tricuspid regurgitation.
“This study’s use ofadvanced cardiovascular imaging, and more specifically 3-D echocardiography, providednew insight into the pathophysiology of tricuspid regurgitation and a goodunderstanding as to why current surgical treatments for tricuspid regurgitationare not good enough,” explained Lerakis. “I believe this study will change thefocus and direction of future surgical therapies for tricuspid regurgitationonly to make them better and more durable.”
Based on the findings of this study, said Lerakis, future surgical therapiesshould not only be focused on the tricuspid annulus, but on the entiretricuspid valve apparatus, including the tricuspid valve papillary muscles andtheir three-dimensional location within the apparatus.
Individuals in the study with left ventricle dilation exhibitedsignificant displacement of one of the papillary muscles and patients with both ventricles dilated hadsignificant displacement of two papillary muscles. Subjects with rightventricle dilation showed significant displacement of all three papillarymuscles.
The researchers also found that patients with a dilated rightventricle were more likely to have a dilated annulus and exhibited the highestpulmonary arterial pressures and highest levels of tricuspid regurgitation. However,not all patients with a dilated right ventricle had significant increases inannulus area, providing evidence that the right ventricle may become dilatedwithout the annulus being affected.
“We think an increase in pulmonary arterial pressure causedgeometric changes in the ventricle, which resulted in alterations to theannulus and papillary muscles,” explainedYoganathan. “The combination of displacement of all three papillarymuscles and annular dilatation may account for the patients with isolated rightventricle dilatation having the largest percentage of severe tricuspid regurgitation.”
Knowing which parameters are responsible for significant tricuspidregurgitation and having a non-invasive imaging technique to measure theseparameters should help clinicians target repairs to the specific cause of an individual’stricuspid leakage, according to Yoganathan.
In future studies, the researchers plan to study papillarymuscle displacements in individuals with specific diseases to see if differentdisease manifestations exhibit different characteristics.
“Although it has long been accepted that pulmonaryhypertension may result in tricuspid regurgitation, this study is one of thefirst to provide a clinical correlation between the two,” said Yoganathan, whois also the Wallace H. Coulter Distinguished Faculty Chair in BiomedicalEngineering. “We want to know whether treating an individual’s pulmonary hypertension,and thus decreasing one’s pulmonary arterial pressure, can reverse thegeometric changes that are causing tricuspid regurgitation and return the annulusand papillary muscles to their original positions.”
Emory University sonographers Jason Higginson, Maria Pernetzand Sharon Howell also contributed to the study.
Research News & Publications Office
Georgia Institute of Technology
75 Fifth Street, N.W., Suite 314
Atlanta, Georgia 30308 USA
Media RelationsContacts: Abby Robinson (abby@innovate.gatech.edu; 404-385-3364) or JohnToon (jtoon@gatech.edu; 404-894-6986)
Writer: AbbyRobinson
News Contact
Abby Robinson
Research News and Publications
abby@innovate.gatech.edu
404-385-3364